Psoriasis
Treatment & Medications
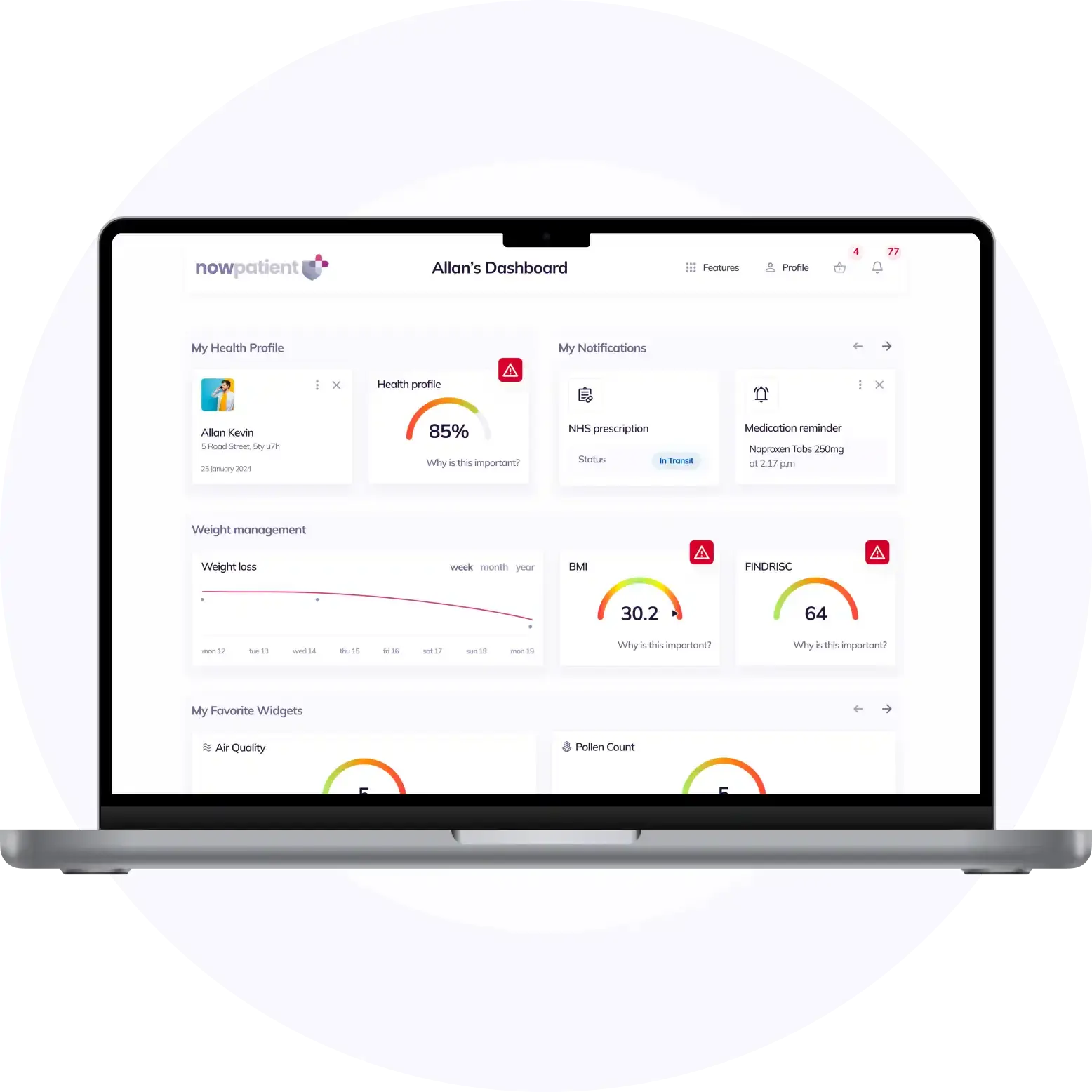
With NowPatient's private treatment plans you can treat Psoriasis safely and easily in a few simple steps. Get started by selecting the available treatments you are interested in below or by hitting the start consultation button.
This content is intended for UK audiences only
Available treatments
Compare treatments
Get started with the right treatment for you
Treatments & Medications
delivery
service

Psoriasis is a chronic skin condition that affects millions of people worldwide. It is characterized by the rapid multiplication of skin cells, rsulting in the build up of scaly, inflamed patches on the skin. While there is no cure for psoriasis, various treatments and lifestyle changes can help manage symptoms and improve quality of life. In this comprehensive guide, we will delve into the causes, symptoms, types, and treatment options for psoriasis.
What is Psoriasis?
Psoriasis is an immune-mediated skin disease that causes inflammation in the body and manifests on the skin. The immune system becomes overactive, resulting in the rapid growth of skin cells. Normally, skin cells go through a cycle of growth, maturation, and shedding in about a month. However, in individuals with psoriasis, this process is significantly accelerated, with skin cells turning over every three to four days. This rapid cell turnover leads to the build up of skin cells on the surface, forming raised plaques.
The exact cause of psoriasis is still not fully understood, but it is believed to involve a combination of genetic and environmental risk factors. It is not contagious and cannot be transmitted from person to person. Psoriasis can occur at any age, but symptoms often appear between the ages of 15 and 25.
Types of Psoriasis
Psoriasis can manifest in various forms, each with its own distinct characteristics. The most common type is plaque psoriasis, which accounts for the majority of cases. Plaque psoriasis presents as raised, red patches of skin covered in silvery-white scales. Other types of psoriasis include guttate psoriasis, pustular psoriasis, inverse psoriasis, and erythrodermic psoriasis. Each type has its own unique symptoms and affects different areas of the body.
- Plaque Psoriasis: This is the most common type of psoriasis, making up 80% of cases according to the American Academy of Dermatology. Symptoms include dry, red skin lesions covered in silver scales. Plaque psoriasi normally appears on the knees, elbows, scalp and lower back, but may appear anywhere on your body. Plaques can be sore, itchy, or both. In more severe cases, skin around the joints may crack and bleed
- Guttate Psoriasis: Guttate psoriasis causes small drop-shaped sores, less than 1cm, on your arms, legs, chest, and scalp. Guttate psoriasis normally disappears after a few weeks, but some people may go on to develop plaque psoriasis. Guttate Psoriasis may occur after a strep throat infection and is more prevalent in children, teenagers and young adults
- Pustular Psoriasis: Characterized by pus-filled blisters surrounded by red skin, primarily affecting the hands and feet. Pustular psoriasis is a rarer type of psoriasis. Different types of pustular psoriasis affect different parts of the body
- Inverse Psoriasis: Presents as large smooth red patches in skin folds or creases in your skin, such as beneath the armpits, between the buttocks, under breasts or in the groin. Inverse psoriasis can be made worse by sweating and friction and can be quite uncomfortable in hot weather
- Erythrodermic Psoriasis: A rare and severe form of psoriasis that covers large areas of the body and requires immediate medical attention. Erythrodermic Psoriasis causes discoloration of the skin and the shedding of scales on sheets. It may be triggered by bad sunburn, certain medications, infections, and stopping psoriasis treatment
- Scalp psoriasis: This may occur on the whole or part of your scalp. Scalp psoriasis may cause red patches of skin covered in thick silvery-white scales. Scalp psoriasis can feel extremely itchy, or cause no discomfort at all. In more serious cases it can cause hair loss. This however, is usually only temporary
- Nail psoriasis: Nail psoriasis affects about half of all people with psoriasis, causing your nails to become discoloured, develop tiny dents or pits, or grow abnormally. Nails can become loose and detach from your nail bed. In more severe cases, your nails may crumble
- Palmoplantar pustular psoriasis: This type of psoriasis causes pustules to appear on the soles of your feet and the palms of your hands. The pustules form circular brown, scaly spots, which peel off. The pustules may reappear after a few days or weeks
- Acropustulosis: Here, pustules appear on your fingers and toes. These then burst, leaving areas bright red. These areas may then ooze or become scaly. Acropustulosis may also lead to painful nail deformities
- Erythrodermic psoriasis: This is a rare form of psoriasis that can affect nearly all the skin on the body, causing intense itching or burning. This type of psoriasis can cause your body to lose fluid and proteins, leading to infections, malnutrition, dehydration, hypothermia and heart disease
Symptoms of Psoriasis
The symptoms of psoriasis can vary from person to person and depend on the type and severity of the condition. Common symptoms include:
- Raised, inflamed patches of skin covered in scales
- Itching, burning, or stinging sensations
- Dry, cracked skin that may bleed
- Nail abnormalities, such as pitting or ridges
- Joint pain and stiffness (in cases of psoriatic arthritis)
The severity of symptoms can range from mild to severe, and they may come and go in cycles. It is essential to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Causes of Psoriasis
Psoriasis is considered an autoimmune disease, meaning it involves an abnormal immune response. The exact triggers for this immune dysfunction are not fully understood, but research suggests that genetics and environmental factors play significant roles.
- Genetics: Family history of psoriasis increases the likelihood of developing the condition. Certain genes related to immune system function are thought to contribute to the development of psoriasis
- Immune system dysfunction: In individuals with psoriasis, the immune system mistakenly attacks healthy skin cells, leading to inflammation and rapid cell turnover
- Environmental factors: Infections, such as streptococcal infections, can trigger or exacerbate psoriasis symptoms. Other factors, such as stress, skin injuries, smoking, and obesity, may also contribute to the development or worsening of psoriasis
- Other medications: Beta blockers, other high high blood pressure drugs, antimalarials, lithium and other mood stabilizers, NSAIDs and antibiotics
Who is at risk?
Psoriasis can affect people of all ages and ethnic backgrounds, but certain factors may increase the risk of developing the condition and flare-ups. These include:
- Family history of psoriasis: Having a close relative with psoriasis increases the likelihood of developing the condition
- Genetics: Certain genetic variations have been associated with an increased susceptibility to psoriasis
- Age: While psoriasis can occur at any age, it most commonly appears between 15 and 25 years old
- Ethnicity: Psoriasis is more prevalent in certain ethnic groups, with higher rates observed in individuals of European descent
- Lifestyle factors: Smoking, obesity, and certain medications can increase the risk or severity of psoriasis
Diagnosing Psoriasis
Diagnosing psoriasis typically involves a thorough physical examination and a review of medical history. Your healthcare provider will examine your skin, nails, and scalp for characteristic signs of psoriasis, such as red, scaly patches or nail abnormalities. In some cases, a skin biopsy may be performed to confirm the diagnosis.
It is important to inform your healthcare provider about any symptoms, family history of psoriasis, and any potential triggers that may have preceded the onset or worsening of symptoms. This information will help guide the diagnosis and treatment plan.
Treatment options
While there is no cure for psoriasis, various treatment options can help manage symptoms, reduce inflammation, and improve quality of life. The choice of treatment depends on the type and severity of psoriasis, as well as individual factors such as age, overall health, and personal preferences. Mild psoriasis can be treated with creams or ointments, while moderate and severe psoriasis may need treatment with tablets, injections, or phototherapy. Treatment options include:
- Topical treatments: Vitamin D creams, topical corticosteroid (steroid) ointments, and lotions containing retinoids (vitamin A derivative) applied directly to the affected skin to reduce inflammation and promote healing
- Phototherapy (light therapy): Controlled exposure to ultraviolet light to slow down skin cell turnover and reduce inflammation
- Systemic medications: Prescription medications that target the immune system, (such as methotrexate) and reduce inflammation throughout the body
- Biologics and small molecule inhibitors: Advanced therapies that specifically target molecules involved in the immune response, providing targeted relief from psoriasis symptoms
- Lifestyle modifications: Adopting healthy habits, such as managing stress, maintaining a healthy weight, and avoiding triggers, can help improve symptoms and overall well-being
It is important to work closely with a healthcare provider to develop an individualized treatment plan that best suits your needs.
Lifestyle changes for Psoriasis management
In addition to medical treatments, certain lifestyle changes can help manage psoriasis symptoms and improve overall well-being. These include:
- Moisturizing the skin regularly to prevent dryness and reduce itching
- Avoiding triggers, such as stress, skin injuries, and certain medications
- Practicing good skin hygiene to minimize the risk of infections
- Maintaining a healthy weight through a balanced diet and regular exercise
- Managing stress through relaxation techniques, exercise, and seeking support from loved ones or support groups
- Protecting the skin from excessive sun exposure and using sunscreen with a high sun protection factor (SPF)
Psoriasis and mental health
Living with psoriasis can have a significant impact on mental health and well-being. The visible nature of the condition and the associated symptoms, such as itching and discomfort, can lead to feelings of self-consciousness, embarrassment, and low self-esteem. It is essential to address these emotional challenges and seek support from healthcare professionals, support groups, or mental health counselors.
Additionally, individuals with psoriasis may be at a higher risk of developing mental health conditions, such as anxiety and depression. It is important to be aware of these potential risks and seek appropriate care when needed.
Psoriasis and Psoriatic Arthritis
Psoriatic arthritis is a common complication of psoriasis, affecting up to one-third of individuals with the skin condition. It is characterized by inflammation, pain, stiffness, and swelling in the joints, often accompanied by skin and nail changes. Early diagnosis and treatment are crucial to prevent joint damage and preserve joint function.
Treatment options for psoriatic arthritis include medications to reduce inflammation, physical therapy, exercise, and lifestyle modifications. A multidisciplinary approach involving rheumatologists, dermatologists, and other healthcare professionals is often necessary to manage both psoriasis and psoriatic arthritis effectively.
Research and advancements in Psoriasis treatment
Ongoing research continues to uncover new insights into the causes and treatment of psoriasis. Scientists are exploring various pathways in the immune system that contribute to psoriasis development, leading to the development of targeted therapies. Biologic drugs, which specifically target molecules involved in the immune response, have revolutionized psoriasis treatment and offer new hope for individuals with severe or refractory psoriasis.
In addition to medical advancements, researchers are also investigating the impact of lifestyle factors, such as diet, exercise, and stress management, on psoriasis symptoms and overall well-being. These findings may further enhance treatment approaches and improve outcomes for individuals with psoriasis.
Conclusion
Psoriasis is a chronic skin condition characterized by the rapid growth of skin cells, leading to the formation of scaly, inflamed patches. While there is no cure, various treatment options and lifestyle changes can help manage symptoms and improve quality of life. Early diagnosis, appropriate treatment, and a multidisciplinary approach involving healthcare professionals are key to effectively managing psoriasis and its potential complications.
By understanding the causes, symptoms, types, and treatment options for psoriasis, individuals and healthcare providers can work together to develop personalized approaches to managing this chronic condition. With ongoing research and advancements in treatment, there is hope for better outcomes and improved quality of life for those living with psoriasis.
Remember, if you suspect you may have psoriasis or are experiencing any symptoms, consult a healthcare professional for an accurate diagnosis and guidance on the most appropriate treatment plan for your specific needs.
Sources
- NHS psoriasis
- WebMD – Psoriasis
- Cleveland Clinic – Psoriasis guide
- Psoriasis.org – About Psoriasis
- NIH – Psoriasis
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
What is NowPatient
Telehealth and Online Pharmacy
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process