Urinary Incontinence
Treatment & Medications
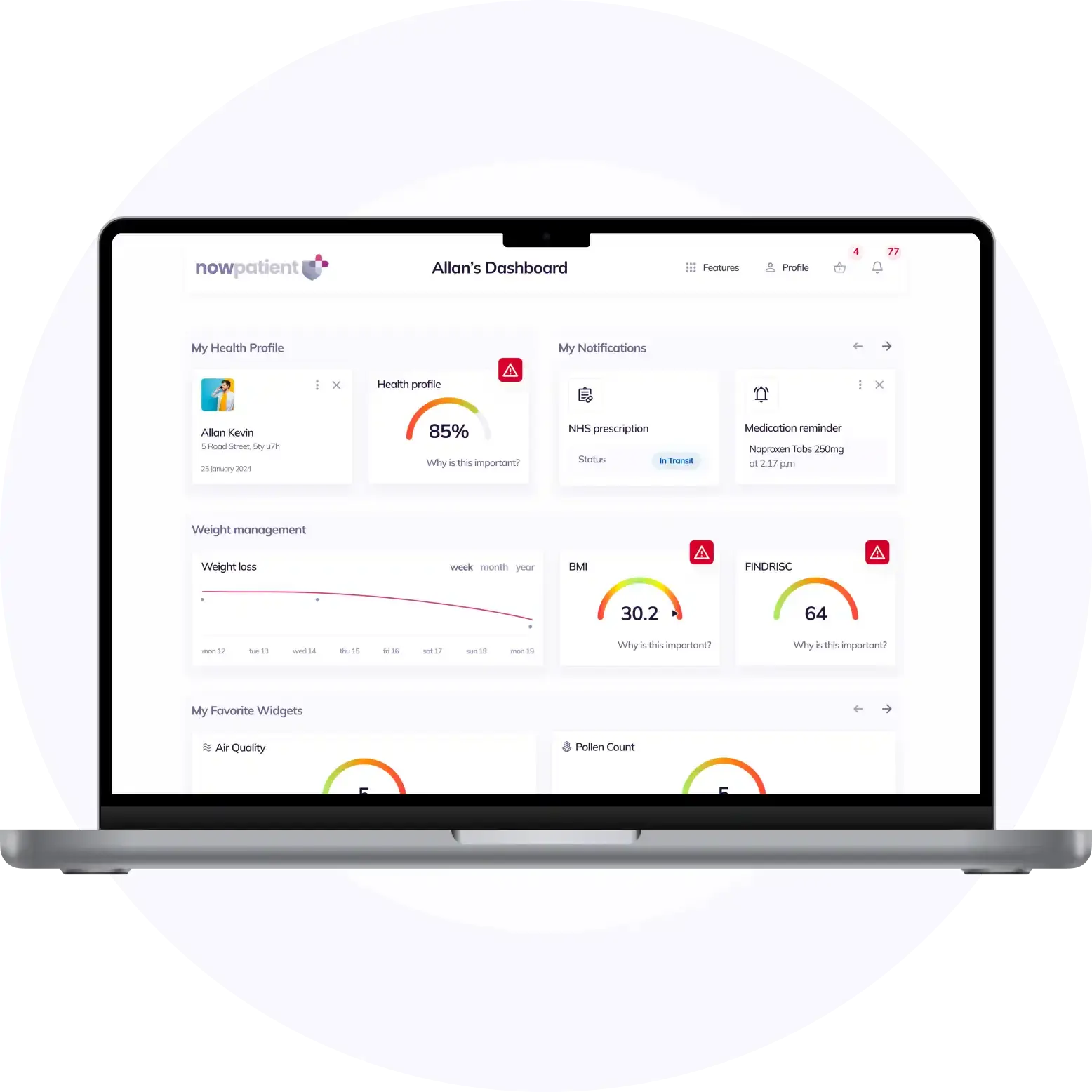
With NowPatient's private treatment plans you can treat Urinary Incontinence safely and easily in a few simple steps. Get started by selecting the available treatments you are interested in below or by hitting the start consultation button.
This content is intended for UK audiences only
Available treatments
Compare treatments
Get started with the right treatment for you
Treatments & Medications
delivery
service

Urinary incontinence, characterized by the unintentional passing of urine, is a condition that affects individuals across the globe, with greater significance in women and the elderly. The occurrence of urinary incontinence is not simply a byproduct of aging and requires consideration for its impact on one’s quality of life and mental well-being. This health concern encompasses various types, such as stress, urge, overflow, functional, mixed, reflex, and total incontinence, each presenting its unique challenges and implications on daily activities.
Beginning with an understanding of the condition and continuing through the exploration of its causes, and examining the symptoms and procedures involved in the diagnosis of urinary incontinence, we will then progress to discussing the management strategies and treatment options that can help mitigate its effects. Furthermore, this article will address strategies for navigating daily life with urinary incontinence, providing you with a comprehensive view that underscores the importance of bladder health.
Understanding urinary incontinence
Understanding the various forms of urinary incontinence is essential for both patients and healthcare providers to manage the condition effectively. Here, we delve into the primary types of urinary incontinence, each with its unique symptoms and challenges:
Stress Incontinence (stress urinary incontinence):
- Occurs when physical activities like coughing, sneezing, or exercising put pressure on the bladder, leading to involuntary urine leakage
- Common in women, especially those who have experienced childbirth or menopause
- Management often includes pelvic floor exercises and lifestyle modifications to reduce bladder pressure
Urge Incontinence:
- Characterized by a sudden, intense urge to urinate followed by involuntary urine leakage, often with little warning
- Can be associated with conditions affecting the bladder’s ability to hold urine, such as urinary tract infections or neurological disorders
- Treatment may involve bladder training, medications, or nerve stimulation techniques to improve bladder control
Overflow Incontinence:
- Results from the bladder’s inability to empty completely, causing frequent or constant dribbling of urine
- Often related to a blockage or obstruction in the bladder or urethra, or nerve damage affecting bladder function
- Catheterization or surgery may be necessary in some cases to alleviate symptoms
Total Incontinence:
- Involves continuous urine leakage or frequent uncontrolled urination due to severe bladder dysfunction
- Can stem from anatomical abnormalities or significant damage to the urinary system
- Management strategies are typically more complex and may include surgical interventions or specialized containment devices
Mixed incontinence:
- When you may have symptoms of both urge and stress incontinence
Each type of incontinence has distinct symptoms and causes, necessitating a personalized approach to treatment. It’s crucial to recognize that urinary incontinence is a common issue, affecting millions of people worldwide. By understanding the specific type of incontinence a person is experiencing, healthcare professionals can tailor treatment strategies to improve bladder control and enhance quality of life.
Incorporating lifestyle changes, such as maintaining a healthy weight and avoiding bladder irritants, can also play a role in managing symptoms. For individuals living with urinary incontinence, understanding the condition is the first step towards regaining control and minimizing its impact on daily life.
Causes of urinary incontinence
The factors contributing to urinary incontinence are multifaceted, ranging from physiological changes to lifestyle influences. Understanding these causes is crucial for addressing the condition effectively:
- Age-related changes: As individuals age, the muscles that support bladder control can weaken, and the nerves that signal the need to urinate may not work as well. This can lead to involuntary leakage of urine, particularly in the elderly population. Age-related changes in the urinary system are a significant contributor to urinary incontinence
- Pregnancy and childbirth: These life stages exert extra pressure on the bladder and pelvic floor muscles, potentially leading to stress incontinence. The act of childbirth can further compromise the integrity of the muscles and nerves responsible for urination control. Pregnancy and childbirth are pivotal moments that can increase the likelihood of urinary incontinence
- Menopause: The decline in estrogen levels during menopause can weaken the urinary tract muscles, contributing to incontinence. This hormonal change is a pivotal factor in the development of urinary incontinence during the postmenopausal phase. Menopause is a natural transition that can inadvertently affect bladder control
- Obesity: Carrying excess weight increases pressure on the bladder, which can lead to stress incontinence. Managing one’s weight can be a proactive step in reducing the symptoms associated with this condition. Obesity is a modifiable risk factor for urinary incontinence
- Family history: Genetics may play a role in predisposing individuals to urinary incontinence, indicating the importance of understanding one’s family medical history. Family history can be a telling indicator of one’s risk for developing urinary incontinence
- Underlying medical conditions: A range of health conditions, including neurological disorders such as multiple sclerosis, diabetes, an enlarged prostate gland and urinary tract infections, can impair bladder function. These conditions can disrupt the normal process of storing and releasing urine, leading to incontinence. Underlying medical conditions are critical to consider when diagnosing and treating urinary incontinence
- Medications: Certain medications, notably diuretics, sedatives, and muscle relaxants, may increase the likelihood of urinary incontinence by affecting bladder control. It’s important to review medication side effects with healthcare providers. Medications can be an overlooked source of urinary incontinence
- Lifestyle factors: The consumption of alcohol, caffeine, and certain foods can irritate the bladder, exacerbating urinary incontinence symptoms. Modifying these dietary habits may provide symptomatic relief. Lifestyle factors play a significant role in managing urinary incontinence
- Neural and structural damage: Injury to the neural pathways or damage to the bladder, sphincters, supporting structures, or pelvic floor can result in urinary incontinence. Each of these components plays a vital role in maintaining continence, and their impairment can lead to loss of bladder control. Fortunately, treatment options are available to address these issues and improve symptoms. Neural and structural damage can have a profound impact on urinary function
In summary, the causes of urinary incontinence are diverse and can be influenced by temporary factors such as diet and medication, as well as more persistent conditions like aging, hormonal changes, and physical damage. Addressing these underlying causes is a critical step in the management and treatment of urinary incontinence.
Symptoms and diagnosis
Individuals experiencing symptoms of urinary incontinence should seek medical advice to receive a proper diagnosis. The diagnostic process is multifaceted and typically includes:
Initial consultation: A general practitioner (GP) will conduct a detailed interview to gather information about the patient’s symptoms and medical history. Questions may cover:
- The occurrence of incontinence when coughing or laughing
- Frequency of the urge to urinate, both during the day and at night
- Any difficulties experienced while passing urine
- Current medications that may influence bladder function
- Intake of fluids, alcohol, or caffeine which might affect the bladder
- It is crucial for patients to provide accurate information to help determine the type of urinary incontinence and the best course of treatment.
Physical examination: This may include a stress test to diagnose stress incontinence, where the patient is asked to perform activities that typically trigger urine leakage
Diagnostic tests: The GP may request several tests to further understand the bladder’s condition:
Urinalysis: To check for signs of infection or other underlying conditions
Bladder diary: Patients may need to record their bladder activity for at least 3 days, noting the times they urinate and the amount of urine produced
Postvoid Residual Measurement: To measure the amount of urine left in the bladder after urination
Urodynamic testing: To assess how well the bladder, sphincters, and urethra are storing and releasing urine
Cystoscopy: An examination of the bladder lining and urethra
Pelvic ultrasound: To visualize the pelvic organs and check for abnormalities
These tests help confirm the diagnosis or rule out other conditions that may cause urinary incontinence. For instance, urinary retention can lead to overflow incontinence, which underscores the importance of a thorough evaluation and accurate diagnosis.
It is important to note that urinary incontinence is a common issue, with approximately one in three women and one in eight men experiencing bladder leakage. This prevalence highlights the significance of consulting healthcare professionals for management and treatment options. If you or someone you know is dealing with symptoms of urinary incontinence, do not hesitate to reach out to a healthcare provider for a comprehensive evaluation and personalized care plan.
Managing and treating urinary incontinence
Managing urinary incontinence involves a spectrum of approaches tailored to the individual’s condition, ranging from non-invasive strategies to surgical interventions:
Lifestyle modifications and behavioral therapies:
- Healthy weight: Achieving and maintaining a healthy weight reduces pressure on the bladder and can alleviate symptoms
- Fluid and diet management: Adjusting fluid intake and reducing bladder irritants like caffeine can help manage the condition
- Pelvic floor exercises: Regularly performing exercises, such as Kegels, strengthens the pelvic muscles that control urination
- Bladder training: Techniques to delay urination can gradually increase the bladder’s capacity and improve control
- Incontinence products: A variety of products, from absorbent pads to catheters, provide support and manage leakage
Pharmacological treatments:
- Duloxetine: Boosts muscle tone in the urethra, although side effects such as nausea and dry mouth may occur
- Antimuscarinics: Medications like oxybutynin help control overactive bladder but may cause dry mouth and blurred vision
- Mirabegron: Relaxes the bladder muscle, enhancing its ability to store urine, with potential side effects including urinary tract infections
Surgical Options:
- Colposuspension and sling procedures: Provide long-term solutions for stress incontinence but carry risks like difficulty emptying the bladder and discomfort
- Urethral bulking agents: Offer a less invasive option, though they may be less effective and require repeat treatments
- Artificial urinary sphincter: Especially beneficial for individuals with a penis, this device may lead to temporary discomfort and has a risk of eventually ceasing to function
- Botulinum toxin A injections: Relax the bladder muscles, but could result in difficulty emptying the bladder completely
- Nerve stimulation therapies: Sacral nerve stimulation and posterior tibial nerve stimulation can significantly improve symptoms by enhancing neural signaling
Specialist services and support:
- NHS continence services: Specialist nurses and physiotherapists offer diagnosis, treatment, and support for managing urinary incontinence
It is noteworthy that approximately 80% of those affected by urinary incontinence can see improvement with these treatments. Caregivers managing someone with incontinence may also benefit from implementing increased fluid intake, high-fiber diets, and utilizing incontinence aids. For those seeking specialized care, Johns Hopkins Medicine provides resources for finding experts in the field.
In conclusion, the management and treatment of urinary incontinence are highly individualized. A combination of methods, from lifestyle changes and pelvic floor exercises to medical treatments and surgery, is often necessary, depending on the type and severity of the condition.
Living with urinary incontinence
Living with urinary incontinence can be a significant challenge, but with the right strategies and support, individuals can manage symptoms effectively and maintain a high quality of life. Here are practical tips for day-to-day management:
- Pelvic floor muscle training: Consistent daily exercises can strengthen the pelvic floor muscles, potentially reducing urine leaks. Notably, improvements can be observed after consistent practice over a period of up to three months. For detailed guidance on these exercises, refer to NHS advice on stopping leaks
Lifestyle adjustments:
- Weight management: Losing excess weight can alleviate the pressure on pelvic floor muscles, thus improving or even eliminating symptoms
- Dietary changes: Minimizing the intake of caffeine, alcohol, spicy, and acidic foods can lessen bladder irritation and incontinence episodes
- Fluid intake: Drinking 6 to 8 glasses of fluid daily is essential to avoid dehydration, which can exacerbate incontinence symptoms
- Smoking cessation: Smoking can increase the risk of incontinence due to cough-induced pressure on the bladder, so quitting smoking is beneficial
- Exercise modifications: Opting for low-impact strengthening exercises, such as Pilates, can enhance pelvic floor muscle strength without excessive strain
- Careful lifting: Avoid heavy lifting to prevent strain on pelvic floor muscles; if necessary, engage pelvic floor muscles before lifting
Proactive planning:
- Trigger awareness: Being mindful of personal triggers and planning accordingly, such as knowing the locations of bathrooms, can help manage incontinence effectively
- Incontinence products: Carrying appropriate products can provide security and confidence when out and about
Emotional well-being:
- Open communication: Discussing concerns with partners, family, or friends can offer emotional support and alleviate stress or depression linked to incontinence
- Professional support: Seeking professional help if needed can provide additional strategies and coping mechanisms
- For caregivers: Caregivers are encouraged to seek support, including referrals to local continence services and assessments by a nurse to tailor care plans for those they are caring for. It’s important to address not only the physical needs but also the emotional well-being of the person affected by incontinence. For more insights on caring for someone with incontinence, explore resources provided by Better Health Channel on incontinence tips for carers.
Incorporating these strategies into daily routines can significantly reduce the impact of urinary incontinence on daily activities. It’s important to remember that while urinary incontinence can be more common with aging, it is not an inevitable part of getting older and can often be improved with treatment. For further information on managing urinary incontinence and improving bladder health, individuals can consult NHS Inform for comprehensive guidance.
Conclusion
Embracing strategies like lifestyle changes, engaging in tailored therapies, and exploring the wealth of professional support can lead to significant enhancements in one’s quality of life. Navigating this sensitive health issue with educated choices and proactive measures is key, and for those ready to take the next step, further resources and guidance can be found through comprehensive platforms like NHS Inform, poised to equip individuals with the knowledge and support they require.
FAQs
What can be done to treat urinary incontinence?
To alleviate symptoms of urinary incontinence, individuals can adopt several self-help strategies and lifestyle modifications, such as:
- Performing daily pelvic floor exercises
- Quitting smoking
- Engaging in appropriate exercises
- Avoiding heavy lifting
- Losing excess body weight
- Addressing constipation promptly
- Reducing caffeine intake
- Limiting alcohol consumption
What are the different types of urinary incontinence?
Urinary incontinence can be temporary or chronic and is more prevalent in women over 50. There are four main categories of urinary incontinence:
- Urgency incontinence
- Stress incontinence
- Functional incontinence
- Overflow incontinence
How can I improve my bladder control?
Improving bladder control can be achieved by performing pelvic floor muscle exercises, commonly known as Kegel exercises. These exercises strengthen the muscles that support the bladder and help prevent urine leakage during activities such as sneezing, coughing, lifting, laughing, or when you suddenly feel the need to urinate.
Why might someone experience constant urine leakage?
Persistent urine leakage, known as urge incontinence, may result from various conditions ranging from minor, such as infections, to more serious issues like neurological disorders or diabetes. Another type, overflow incontinence, is characterized by frequent or continuous dribbling of urine due to the bladder not emptying fully.
Sources
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
What is NowPatient
Telehealth and Online Pharmacy
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process