Shingles
Treatment & Medications
With NowPatient's private treatment plans you can treat Shingles safely and easily in a few simple steps. Get started by selecting the available treatments you are interested in below or by hitting the start consultation button.
This content is intended for UK audiences only
Available treatments
Compare treatments
Get started with the right treatment for you
Treatments & Medications
delivery
service

Shingles, also known as herpes zoster, is a viral infection that causes a painful rash. It is caused by the varicella-zoster virus (VZV), the same virus that causes chickenpox. After a person has had chickenpox, the virus remains dormant in certain nerves in the body for many years. However, as a person gets older or experiences a weakened immune system, the virus can become reactivated and lead to the development of Shingles. In this comprehensive guide, we will explore the causes, symptoms, treatment, and prevention of shingles.
Understanding Shingles
The primary cause of Shingles is the reactivation of the Varicella-Zoster virus. Shingles is a condition that primarily affects adults, but even children can develop it. The risk of developing Shingles increases with age, and it is more common in individuals over the age of 50. The virus remains inactive in nerve tissues near the spinal cord and brain after a person recovers from chickenpox. However, factors such as stress, a weakened immune system, or advanced age can trigger the reactivation of the virus, leading to Shingles. While the exact reason for reactivation is unclear, it is more common in older adults and individuals with weakened immune systems.
Risk Factors for Shingles
Several factors can increase the risk of developing shingles. Age is a significant risk factor, as Shingles is more common in individuals over the age of 50. Those with weakened immune systems, such as individuals with HIV/AIDS or undergoing cancer treatment, are also at higher risk. Additionally, individuals who have not been vaccinated against chickenpox and have never had the infection are susceptible to developing shingles.
Symptoms of Shingles
The early symptoms of Shingles usually begin with shooting pain, burning, tingling or itching in a specific area of skin. This is often followed by the appearance of a rash, which typically starts as small red spots and progresses to fluid-filled blisters. These blisters eventually scab over and heal within a few weeks. The rash appears localized to one side of your body or face and can be accompanied by other flu-like symptoms such as fever, headache, and an upset stomach. It is important to note that some individuals may experience symptoms without developing a visible skin rash.
Complications of Shingles
While Shingles is generally a self-limiting, non life-threatening condition, it can lead to potential complications, especially in individuals with a weak immune system or the elderly. The most common complication is postherpetic neuralgia (PHN), which causes severe pain in the area where the Shingles rash occurred. PHN can last for weeks, months, or even years after the rash has healed. Other possible complications may include eye problems and vision loss if the rash affects the eye, hearing or balance issues, bacterial skin infections of the rash, and very rarely, neurological complications such as encephalitis if the virus spreads to the brain or spinal cord.
Diagnosing Shingles
The diagnosis of Shingles is typically made based on a physical examination and medical history review by a healthcare provider. Healthcare providers will look for the characteristic rash and inquire about accompanying symptoms such as pain and itching to help confirm the diagnosis. In some cases of Shingles the healthcare provider may collect a small sample of fluid from the blisters for laboratory testing to confirm the presence of the Varicella-Zoster virus. This can help differentiate Shingles from other similar skin conditions.
Treatment Options
While there is no cure for Shingles, there are several treatment options available to alleviate symptoms and promote faster healing. Treatment focuses on symptom management and preventing complications. Antiviral medications, such as acyclovir, famciclovir, and valacyclovir, may be prescribed to help reduce the severity and duration of the infection if taken within a few days of symptom onset. Pain killers, over-the-counter or prescription medications, (nonsteroidal anti-inflammatory drugs such as ibuprofen) may be prescribed to manage the nerve pain and help alleviate discomfort associated with Shingles. It is important to keep the rash clean and dry to prevent bacterial infection. Additionally, topical creams, lotions, as well as cool compresses, and oatmeal baths may also provide relief from itching and discomfort.
Prevention: Vaccination
Vaccination is an effective way to prevent Shingles and reduce the risk of complications. Two vaccines are available: Zostavax and Shingrix. Shingrix is the preferred vaccine and is recommended by healthcare experts for individuals aged 50 and older, due to its high effectiveness in preventing Shingles and PHN. Shingrix may be used, regardless of whether you have had shingles before or have received the previous Zostavax vaccine. The CDC (Centers for Disease Control and Prevention) recommends to administer Shingrix as a two-dose series, with the second dose given 2 to 6 months after the first. Shingrix has shown to be more than 90% effective in preventing shingles and postherpetic neuralgia. Zostavax is an alternative for individuals aged 60 and older, although it is less effective than Shingrix.
Who Should Get Vaccinated
Immunization with the Shingrix vaccine is recommended for individuals aged 50 and older, regardless of whether they have had shingles in the past. It is also recommended for those who have previously received the Zostavax vaccine. The vaccine is generally safe for healthy individuals, but certain individuals, such as pregnant or breastfeeding women, those with severe allergies to vaccine components, or individuals with active shingles, should consult with their healthcare provider before getting vaccinated. The risk of Shingles can be reduced in children by using the chickenpox vaccine if the vaccine is given before the child gets chickenpox.
Side Effects and Risks
Serious side effects from shingles vaccines are extremely rare. However, individuals should be aware of potential allergic reactions, such as swelling of the face or throat, difficulty breathing, hives, or a fast heartbeat. It is important to seek immediate medical attention if any of these symptoms occur after receiving the vaccine. The Zostavax vaccine, being a live vaccine, may not be suitable for individuals with weakened immune systems or certain medical conditions. It is important to discuss any concerns or medical history with a healthcare provider before receiving the vaccine.
Additional Measures for Prevention
In addition to vaccination, there are other measures that can help reduce the risk of shingles. Maintaining a healthy lifestyle, managing stress, and practicing good hygiene can support a strong immune system. Avoiding close contact with individuals who have active chickenpox or shingles can also help prevent the spread of the varicella-zoster virus. Good hand hygiene, such as regular handwashing, is essential in reducing the risk of infection.
Frequently Asked Questions about Shingles
Can you get chickenpox more than once?
Yes. Very rarely, a 2nd case of chickenpox can occur. The symptoms of Shingles is usually more severe in adults than in children. Often people that have had chickenpox will be immune for the rest of their lives. The virus however, remains dormant in nerve tissue and may be reactivated later in life due to certain risk factors, causing Shingles.
What does the Shingles rash look like?
Shingles may occur anywhere on your body. It tends to look like a stripe of blisters, wrapping around one side of the body, either on the right or left side of your torso.
How can you prevent the spread of Shingles?
A person with Shingles may pass the virus to anyone who is not immune to chickenpox. This normally occurs through direct contact with open sores of the Shingles rash. If you have Shingles, cover the rash, do not touch or scratch it, and wash your hands often to prevent it from spreading. The risk of the virus spreading is low if the rash is covered. You will no longer be contagious once the rash develops crusts.
What is the best treatment for Shingles?
Early treatment with antiviral medications such as acyclovir, famciclovir, or valacyclovir is recommended. Dermatologists also recommend using pain relief medication such as paracetamol over the counter, or a prescription drug from your doctor. Other treatments to help relieve itching include wet compresses, calamine lotion, and warm oatmeal baths.
What is the main cause of shingles?
Shingles is caused by the Varicella-Zoster virus. This is the same virus that causes chickenpox. This virus stays in the body once you have had chickenpox. The virus may reactivate later in life, causing Shingles.
Is Shingles caused by stress?
Shingles is not caused by stress, but stress may increase your risk of developing Shingles. Severe stress may weaken your immune system, allowing the dormant virus to reactivate.
Do Shingles go away?
No. Shingles does not go away. It remains dormant in the body after you have had chickenpox. You may however, be able to ease your symptoms, while you recover. Shingles symptoms normally improve within 2 to 4 weeks. Speak to your GP if you get symptoms of Shingles.
Conclusion
Shingles is a viral infection that can cause significant pain and discomfort. Understanding the causes, symptoms, treatment options, and prevention strategies of Shingles is crucial for managing the condition effectively. Vaccination, particularly with the Shingrix vaccine, is strongly recommended for individuals aged 50 and older to reduce the risk of developing Shingles and its complications. If you experience symptoms of Shingles or fall into a high-risk category, it is important to consult with a healthcare provider for proper diagnosis and appropriate treatment. By staying informed, taking preventive measures and seeking timely medical attention such as vaccinations, you can reduce the risk of developing Shingles and its associated complications.
Sources
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
What is NowPatient
Telehealth and Online Pharmacy
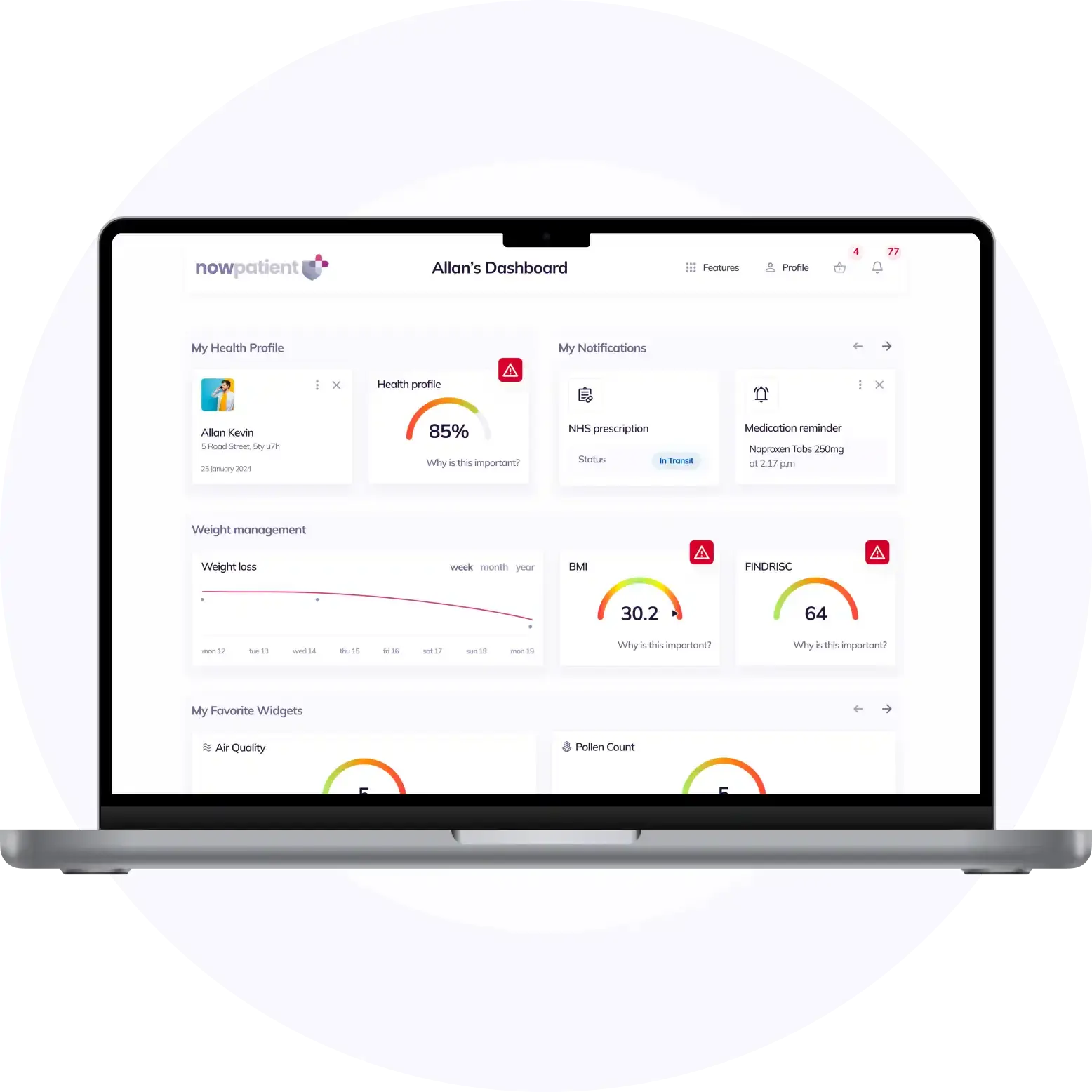
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process