Period Pain
Treatment & Medications
With NowPatient's private treatment plans you can treat Period Pain safely and easily in a few simple steps. Get started by selecting the available treatments you are interested in below or by hitting the start consultation button.
This content is intended for UK audiences only
Available treatments
Compare treatments
Get started with the right treatment for you
Treatments & Medications
delivery
service

Menstrual pain, also known as dysmenorrhea, is a common issue that many women experience during their reproductive years. It can range from mild discomfort to debilitating pain that interferes with daily activities. Understanding the causes, types, and effective management strategies for menstrual pain is essential for women’s health and well-being. In this comprehensive guide, we will answer the most frequently asked questions about menstrual cramps and provide valuable insights into its various aspects. So, let’s dive in and explore everything you need to know about menstrual pain.
What is Menstrual pain?
Menstrual pain, scientifically known as dysmenorrhea, refers to the discomfort or pain experienced by women during their menstrual cycle. It is a prevalent condition affecting more than half of women worldwide, typically occurring one to two days before or during menstruation. Menstrual pain can range from mild cramping to severe, debilitating pain that interferes with daily activities.
Definition and prevalence
Menstrual pain, or dysmenorrhea, is the medical term used to describe the pain associated with a woman’s menstrual period. It is estimated that over 50% of women experience menstrual pain to some degree during their reproductive years. This pain can vary in intensity and duration, and its impact on daily life can range from mild inconvenience to significant disruption.
Primary and Secondary Dysmenorrhea: Dysmenorrhea is classified into two types: primary and secondary. Primary dysmenorrhoea refers to menstrual pain that is not caused by any underlying medical condition. It usually starts during adolescence and improves with age or after childbirth. Secondary dysmenorrhoea, on the other hand, is menstrual pain resulting from an underlying condition, such as endometriosis or uterine fibroids. It typically presents later in life and tends to worsen over time.
Causes of Menstrual Pain
Understanding the causes of menstrual pain is crucial for effective management. Several factors contribute to the development of menstrual pain, including the production of prostaglandins and underlying medical conditions.
Prostaglandins and uterine contractions
The primary cause of menstrual pain is the release of prostaglandins, natural chemicals produced in the lining of the uterus. Prostaglandins play a crucial role in triggering uterine contractions necessary for shedding the uterine lining during menstruation. However, an excess amount of prostaglandins can lead to increased intensity and duration of uterine contractions, resulting in period pain and discomfort.
Other underlying conditions
In addition to prostaglandins, several underlying medical conditions can contribute to menstrual pain. These conditions include:
- Endometriosis: A condition where the tissue similar to the lining of the uterus grows outside the uterus, causing inflammation, pain, and sometimes the formation of scar tissue
- Adenomyosis: The presence of endometrial tissue within the muscular wall of the uterus, leading to painful periods and heavy periods
- Uterine fibroids: Non-cancerous growths that develop in or on the uterus, potentially causing pain and heavy menstrual bleeding
- Pelvic inflammatory disease (PID): An infection of the womb, ovaries and fallopian tubes, often resulting from sexually transmitted infections (STIs), which can cause pelvic pain and discomfort
- Cervical stenosis: Narrowing of the cervix, which can impede the flow of menstrual blood and cause pain
- Irregular periods and heavy bleeding
- Intrauterine device (IUD) may also cause period pain, especially during the first 3 to 6 months
Identifying and addressing these underlying conditions is essential for effective management of menstrual pain. Consultation with a healthcare provider and appropriate diagnostic tests are necessary to determine the cause of menstrual pain and develop an individualized treatment plan.
Types of Menstrual Pain
Menstrual pain can be classified into two main types: primary dysmenorrhea and secondary dysmenorrhea. Understanding the characteristics and differences between these types is crucial for proper diagnosis and treatment.
Primary Dysmenorrhea
Primary dysmenorrhea refers to menstrual pain that occurs without any underlying medical condition. It is considered a normal physiological process associated with the menstrual cycle. Primary dysmenorrhea typically starts during adolescence with the onset of menstruation and tends to improve with age or after childbirth.
The pain experienced in primary dysmenorrhea is primarily due to the release of prostaglandins, which cause increased uterine contractions. The intensity and duration of pain vary among individuals, ranging from mild cramping to severe, debilitating pain. Other symptoms associated with primary dysmenorrhea may include nausea, fatigue, headache, and diarrhea.
Secondary Dysmenorrhea
Secondary dysmenorrhea refers to menstrual pain that is caused by an underlying medical condition. Unlike primary dysmenorrhea, secondary dysmenorrhea typically presents later in life and tends to worsen over time. The pain experienced in secondary dysmenorrhea is often more severe and may be accompanied by additional symptoms specific to the underlying condition.
Underlying conditions that can cause secondary dysmenorrhea include endometriosis, adenomyosis, uterine fibroids, pelvic inflammatory disease (PID), and cervical stenosis. Identifying and treating the underlying cause is essential for managing secondary dysmenorrhea effectively.
Identifying Menstrual Pain
Recognizing the signs and symptoms of menstrual pain is crucial for proper diagnosis and effective management. While some degree of discomfort during menstruation is normal, severe or persistent pain may require medical attention.
Signs and symptoms
The signs and symptoms of menstrual pain can vary among individuals. Common manifestations include:
- Cramping pain in the lower abdomen or pelvis
- Dull or throbbing pain that may radiate to the lower back or thighs
- Back pain that starts a few days before or during menstruation and lasts for several days
- Nausea, bloating, vomiting, or diarrhea
- Headache or dizziness
- Fatigue or tiredness
- Mood swings or irritability
Differentiating from other conditions
It is important to differentiate menstrual pain from other conditions that can cause similar symptoms. Some conditions that may mimic menstrual pain include:
- Pelvic inflammatory disease (PID)
- Ovarian cysts
- Urinary tract infections (UTIs)
- Irritable bowel syndrome (IBS)
- Endometriosis
If you experience severe or persistent pain that significantly affects your daily life or if your symptoms worsen over time, it is recommended to consult a healthcare provider for further evaluation and appropriate management.
Seeking medical help
Knowing when to seek medical help for menstrual pain is crucial for timely diagnosis and treatment. While mild discomfort during menstruation is common, certain signs and symptoms warrant a consultation with a healthcare provider.
When to consult a healthcare provider
You should consider consulting a healthcare provider if you experience any of the following:
- Severe or debilitating pain that interferes with daily activities
- Pain that is not relieved by over-the-counter pain medications
- Symptoms that worsen over time or become progressively more severe
- Persistent pain outside of the menstrual period
- Unusual vaginal bleeding or discharge
- Other concerning symptoms, such as fever or severe nausea and vomiting
A healthcare provider can perform a thorough evaluation, including a medical history review and physical examination, to determine the cause of your menstrual pain and recommend appropriate treatment options.
Diagnostic tests for Dysmenorrhea
To diagnose the cause of menstrual pain, your healthcare provider may order various diagnostic tests, including:
- Pelvic ultrasound: This imaging test uses sound waves to create images of the reproductive organs, helping identify any structural abnormalities or conditions such as fibroids or cysts
- Magnetic resonance imaging (MRI): In some cases, an MRI may be recommended to obtain detailed images of the pelvic organs, providing further information about suspected conditions like endometriosis
- Laparoscopy: In certain situations, a minimally invasive surgical procedure called laparoscopy may be required for a direct visualization of the pelvic organs. This procedure allows for the diagnosis and treatment of conditions such as endometriosis or adhesions
These diagnostic tests help to identify the underlying cause of menstrual pain and guide the development of an appropriate treatment plan.
Lifestyle changes for Menstrual Pain management
Making certain lifestyle changes can significantly help in managing menstrual pain. Implementing these changes can alleviate symptoms and improve your overall well-being during your menstrual cycle.
Exercise and physical activity
Engaging in regular physical activity and gentle exercise can help reduce menstrual pain. Exercise promotes the release of endorphins, which are natural pain relievers. It also improves blood circulation, reduces muscle tension, and enhances mood. Aim for at least 30 minutes of moderate-intensity aerobic exercise, such as brisk walking or cycling, on most days of the week.
Stress reduction techniques
Stress can exacerbate menstrual pain symptoms. Practicing stress reduction techniques, such as deep breathing exercises, meditation, yoga, or mindfulness, can help alleviate pain and promote relaxation. Incorporate these techniques into your daily routine, especially during your menstrual period.
Sleep and rest
Adequate sleep and rest are essential for managing menstrual pain. Prioritize getting enough sleep and establish a regular sleep schedule. Create a comfortable sleep environment, practice good sleep hygiene, and consider relaxation techniques before bedtime to improve sleep quality and reduce pain perception.
Dietary considerations
Certain dietary modifications may help alleviate menstrual pain. Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Limit the consumption of processed foods, sugary snacks, caffeine, and alcohol, as they can potentially worsen inflammation and pain symptoms.
Heat therapy
Applying heat to the lower abdomen can provide significant relief from menstrual pain. Use a heating pad, hot water bottle, hot bath, or warm towel and place it on the painful area for 15-20 minutes at a time. Heat helps relax the muscles, improve blood flow, and reduce cramping.
Incorporating these lifestyle changes into your routine can contribute to better management of menstrual pain and overall well-being.
Over-the-counter medications for Menstrual Pain
Over-the-counter (OTC) medications can effectively alleviate menstrual pain and discomfort. Painkillers such as non-steroidal anti-inflammatory drugs (NSAIDs) and paracetamol are commonly recommended for pain relief during menstruation.
Non-steroidal anti-Inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen, naproxen sodium, and aspirin, are effective in reducing menstrual pain by inhibiting the production of prostaglandins. These medications help relieve inflammation, reduce uterine contractions, and alleviate pain. It is important to follow the recommended dosage instructions and consult a healthcare provider if you have any medical conditions or are taking other medications to ensure their safe and proper use.
Effectiveness and safety considerations
NSAIDs are generally considered safe and effective for most women when used as directed. However, they may not be suitable for everyone, especially those with certain medical conditions or allergies. It is important to read and follow the instructions on the packaging, and if you have any concerns or questions, consult a healthcare provider.
Hormonal birth control as a treatment option
Hormonal birth control methods can provide effective relief from menstrual pain. They work by regulating hormone levels and reducing the intensity of uterine contractions.
Combined oral contraceptives
Combined oral contraceptives, commonly known as birth control pills, contain both estrogen and progestin hormones. These hormones help regulate the menstrual cycle, reduce the production of prostaglandins, and alleviate menstrual pain. Consult a healthcare provider to determine whether combined oral contraceptives are suitable for you and to discuss the potential benefits and risks.
Progestin-only methods
Progestin-only birth control methods, such as the mini-pill, hormonal IUD, or contraceptive implant, can also be effective in managing menstrual pain. They work by thinning the lining of the uterus, reducing the production of prostaglandins, and suppressing ovulation. These methods may be recommended for women who cannot take estrogen-containing contraceptives or prefer progestin-only options.
Effectiveness and side effects
Hormonal birth control methods are generally effective in reducing menstrual pain. However, they may have potential side effects, and their suitability varies among individuals. It is important to discuss your medical history, preferences, and any concerns or side effects with a healthcare provider to determine the most appropriate birth control method for you.
Alternative and complementary therapies
In addition to conventional treatments, alternative and complementary therapies can be considered as adjunctive options for managing menstrual pain. These therapies may help alleviate symptoms and improve overall well-being.
Herbal supplements and vitamins
Certain herbal supplements and vitamins have been suggested to have potential benefits in reducing menstrual pain. Examples include:
- Vitamin B1 (thiamine): Thiamine supplementation may alleviate menstrual pain, although more research is needed to establish its effectiveness
- Magnesium: Some studies suggest that magnesium supplementation may help reduce menstrual pain, although further research is required to confirm its efficacy
While herbal supplements and vitamins may be considered as complementary options, it is important to consult a healthcare provider before starting any new supplement, as they can interact with other medications and have potential side effects.
Acupuncture and acupressure
Acupuncture and acupressure have shown promise in reducing menstrual pain. These traditional Chinese medicine techniques involve the stimulation of specific points on the body to promote pain relief and overall well-being. Several studies suggest that acupuncture and acupressure may help alleviate menstrual pain, although more research is needed to determine their efficacy.
It is important to seek the services of a qualified and experienced acupuncturist or acupressure practitioner and discuss potential benefits and risks before undergoing these therapies.
Surgical interventions for Menstrual Pain
In cases where conservative treatments are ineffective or when menstrual pain is caused by specific underlying conditions, surgical interventions may be considered.
Procedures for endometriosis
Endometriosis, a condition where endometrial tissue grows outside the uterus, can cause severe menstrual pain. In cases where conservative management fails, surgical interventions may be necessary. These procedures aim to remove or destroy the endometrial tissue and any associated adhesions. The specific surgical approach depends on the extent and severity of the endometriosis and may include laparoscopy, excision, or ablation techniques.
Uterine artery embolization
Uterine artery embolization (UAE) is a minimally invasive procedure used to treat menstrual pain caused by uterine fibroids. During UAE, small particles are injected into the blood vessels supplying the fibroids, blocking their blood flow and causing them to shrink. This procedure can alleviate pain and reduce the size of fibroids without the need for surgery.
Hysterectomy as a last resort
In rare cases where other treatment options have failed and severe menstrual pain persists, a hysterectomy may be considered. Hysterectomy involves the complete removal of the uterus and can provide permanent relief from menstrual pain. However, it is a major surgical procedure that has significant implications for fertility and should only be considered as a last resort after careful consideration and consultation with a healthcare provider.
Self-care and home remedies
In addition to medical treatments, several self-care practices and home remedies can provide relief from menstrual pain. These simple measures can be incorporated into your daily routine to complement other treatment strategies.
Relaxation techniques
Practicing relaxation techniques, such as deep breathing exercises, meditation, or progressive muscle relaxation, can help reduce stress and alleviate menstrual pain. Find a quiet and comfortable space, and dedicate a few minutes each day to these techniques to promote relaxation and pain relief.
Dietary modifications
Certain dietary modifications may help alleviate menstrual pain. Increase your intake of foods rich in omega-3 fatty acids, such as fatty fish, flaxseeds, and walnuts, as they possess anti-inflammatory properties. Additionally, consuming foods high in calcium, such as dairy products, leafy greens, and fortified plant-based alternatives, may help reduce muscle cramping.
Heat therapy
Applying heat to the lower abdomen can provide significant relief from menstrual pain. Use a heating pad, hot water bottle, or warm towel and place it on the painful area for 15-20 minutes at a time. Heat helps relax the muscles, improve blood flow, and reduce cramping.
Over-the-counter pain relief
Over-the-counter pain relievers, such as acetaminophen or NSAIDs, can be used to alleviate mild to moderate menstrual pain. Follow the recommended dosage instructions and consult a healthcare provider if you have any concerns or medical conditions.
When to seek urgent medical attention
While most cases of menstrual pain are normal and can be managed with self-care measures and medical treatments, certain situations require immediate medical attention. Recognizing potential red flags and emergency situations is crucial for timely intervention.
Red flags
Seek urgent medical attention if you experience any of the following:
- Severe or unbearable pain that is not relieved with over-the-counter pain medications
- Excessive vaginal bleeding, such as soaking through a pad or tampon within an hour
- Fainting or lightheadedness
- High fever and chills
- Severe nausea or vomiting
- Signs of infection, such as pelvic pain and fever
Emergency situations
In rare cases, severe menstrual pain may be a sign of a medical emergency. Seek immediate medical attention or call emergency services if you experience:
- Sudden and severe abdominal pain
- Fainting or loss of consciousness
- Rapid heartbeat or palpitations
- Difficulty breathing
These symptoms may indicate a potentially life-threatening condition that requires urgent medical intervention.
In conclusion, understanding and effectively managing menstrual pain is crucial for women’s health and well-being. By recognizing the causes, types, and available treatment options, women can take proactive steps to alleviate pain and improve their quality of life during menstruation. If you experience severe or persistent menstrual pain, consult a healthcare provider for proper evaluation and personalized treatment recommendations. Remember, you don’t have to suffer in silence—there are effective strategies to manage and overcome menstrual pain.
Sources
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
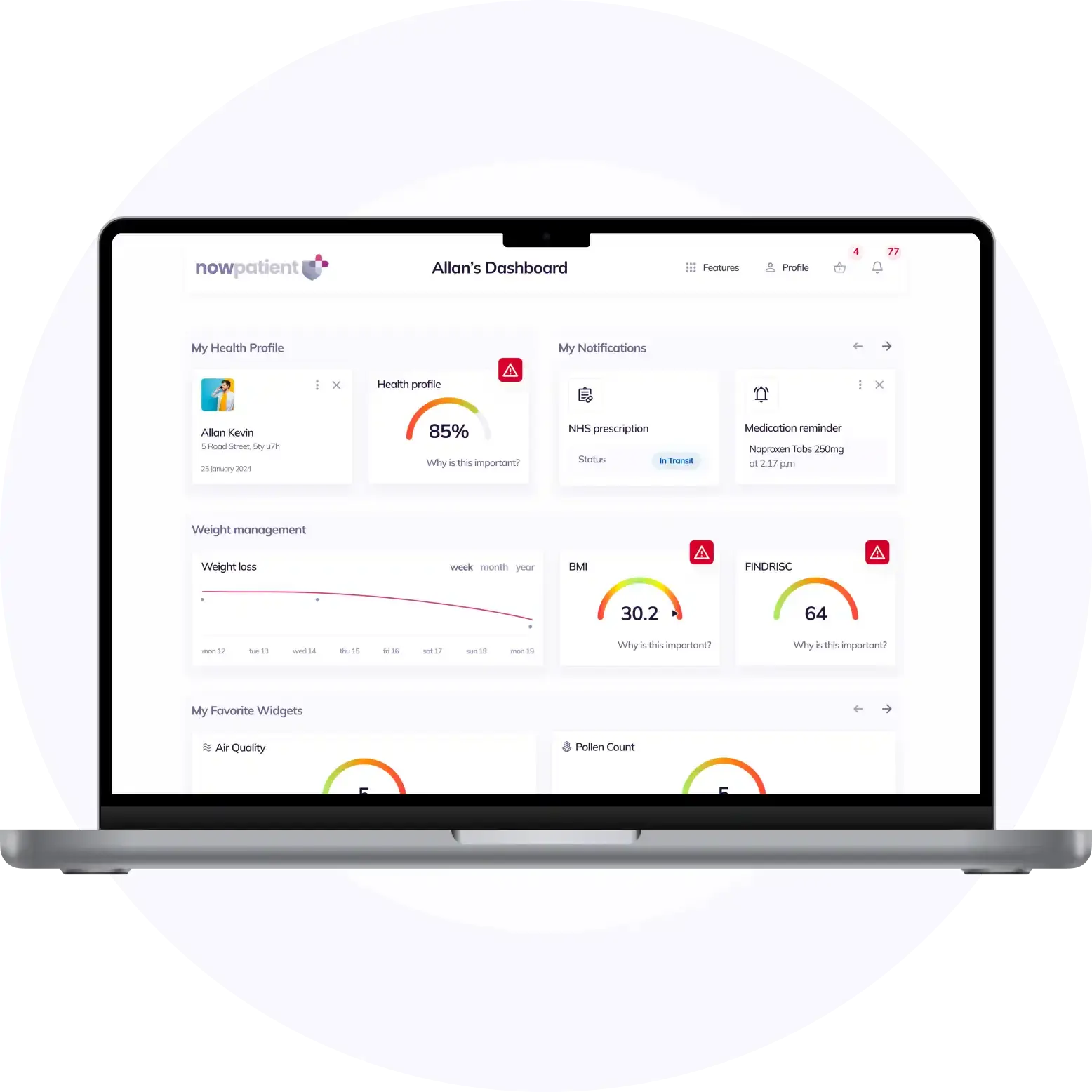
What is NowPatient
Telehealth and Online Pharmacy
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process