Psoriasis
Treatments & Medications
Is the cost of your Psoriasis medication too expensive or unaffordable?
You may qualify for programs where you can pay as little as $0 per fill, subject to income and insurance status.
This content is intended for US audiences only

Psoriasis is a chronic inflammatory skin condition that affects millions of people worldwide. Here, we aim to provide you with a comprehensive overview of psoriasis, including its definition, symptoms, causes, and management strategies. By understanding the complexities of psoriasis, individuals and healthcare professionals can better navigate this condition, promote effective treatment, and improve the quality of life for those affected by it.
What is the definition of psoriasis?
Psoriasis is a chronic autoimmune disorder characterized by the rapid turnover of skin cells, resulting in the formation of thickened, scaly patches on the skin’s surface. It is a non-contagious condition that primarily affects the skin but can also involve joints in some cases. Psoriasis is characterized by an abnormal immune response in which T-cells, a type of white blood cell, mistakenly attack healthy skin cells. This immune dysfunction leads to an accelerated production of new skin cells, causing the accumulation of cells on the skin’s surface and the development of raised, red patches covered with silvery-white scales. Psoriasis is a chronic condition with periods of flare-ups and remission, and it can vary in severity from mild to severe. Proper diagnosis and management by healthcare professionals, such as dermatologists, are essential for effectively treating and controlling psoriasis.
What are the different types of psoriasis?
Plaque psoriasis
Plaque psoriasis is the most common form, accounting for about 80-90% of all psoriasis cases. It is characterized by raised, red patches called plaques covered with silvery-white scales. These plaques often appear on the elbows, knees, scalp, and lower back, but can occur anywhere on the body.
Guttate Psoriasis
Guttate psoriasis is characterized by small, dot-like lesions that are red or pink in color. These lesions are typically widespread on the trunk, limbs, and scalp. Guttate psoriasis often occurs after a bacterial or viral infection, such as strep throat.
Inverse psoriasis
Inverse psoriasis affects skin folds and appears as smooth, red, and inflamed patches. Common areas affected include the armpits, groin, under the breasts, and in skin folds around the genitals and buttocks. Inverse psoriasis can be worsened by friction and sweating.
Pustular psoriasis
Pustular psoriasis is characterized by small, pus-filled blisters surrounded by red skin. The blisters may appear on localized areas of the body or be widespread. Pustular psoriasis can be accompanied by symptoms such as fever, chills, itching, and fatigue.
Erythrodermic psoriasis
Erythrodermic psoriasis is a rare but severe form of psoriasis that can affect the entire body. It causes widespread redness, itching, and shedding of the skin. The skin may appear fiery red and can be extremely itchy and painful.
Nail psoriasis
Nail psoriasis affects the nails, causing changes such as pitting, discoloration, thickening, crumbling, or separation from the nail bed. Nail psoriasis can be associated with other forms of psoriasis or occur independently.
What are the causes and triggers of psoriasis?
The exact cause of psoriasis is not fully understood, but it is believed to involve a combination of genetic, immune system, and environmental factors. Here are the main causes and triggers associated with psoriasis:
Genetic factors
Family History: Having a family history of psoriasis increases the likelihood of developing the condition. Certain genetic variations, particularly in immune-related genes, can contribute to an individual’s susceptibility to psoriasis
Immune system dysfunction
Abnormal Immune Response: Psoriasis is considered an autoimmune disorder, in which the immune system mistakenly attacks healthy skin cells. T-cells, a type of white blood cell, become overactive and trigger inflammation, leading to rapid skin cell growth
Environmental factors
- Infections: Certain infections, particularly streptococcal infections (such as strep throat), can trigger or exacerbate psoriasis in susceptible individuals
- Injury to the skin: Trauma, cuts, scratches, or burns to the skin may trigger the development of psoriasis in specific areas, a phenomenon known as the Koebner phenomenon
- Medications: Some medications, such as certain antimalarial drugs, beta-blockers, lithium, and non-steroidal anti-inflammatory drugs (NSAIDs), can worsen or trigger psoriasis symptoms in susceptible individuals
- Stress: psychological stress or emotional trauma can potentially exacerbate psoriasis or trigger flare-ups in some individuals
- Smoking and alcohol: Both smoking and excessive alcohol consumption have been associated with an increased risk of developing psoriasis and worsening symptoms
Hormonal factors
Hormonal changes, such as during puberty, pregnancy, or menopause, can impact psoriasis symptoms in some individuals
Other Factors
- Obesity: Obesity is a risk factor for psoriasis, and individuals with psoriasis may experience more severe symptoms if they are overweight or obese
- Climate and Weather: Cold weather, dry air, and low humidity levels can worsen psoriasis symptoms, while sunlight and warmer weather can help improve symptoms for some individuals
It’s important to note that triggers can vary from person to person, and not everyone with psoriasis will have the same triggers. Identifying and avoiding triggers, when possible, can help reduce the frequency and severity of psoriasis flare-ups. However, managing psoriasis often requires a multifaceted approach involving proper skincare, lifestyle adjustments, stress management, and medical treatment. Consulting with a healthcare professional, such as a dermatologist, can provide personalised guidance for managing psoriasis triggers effectively.
What is the pathophysiology of psoriasis?
The pathophysiology of psoriasis involves a complex interplay of genetic, immune system, and environmental factors. Here is an overview of the key elements involved in the pathophysiology of psoriasis:
Genetic predisposition
Genetic factors play a significant role in the development of psoriasis. Certain genetic variations, particularly in immune-related genes, are associated with an increased risk of developing the condition. Psoriasis has a strong genetic component, as it tends to run in families.
Psoriasis immune system dysfunction
- Psoriasis is considered an autoimmune disorder, characterized by an abnormal immune response. In individuals with psoriasis, the immune system mistakenly identifies healthy skin cells as foreign invaders and triggers an inflammatory response
- T-cells, a type of white blood cell, are overactive in psoriasis and produce an excess of inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-alpha), interleukin-17 (IL-17), and interleukin-23 (IL-23)
- These cytokines promote an inflammatory cascade, leading to the proliferation of skin cells and the recruitment of other immune cells to the skin, including neutrophils and dendritic cells
Hyperproliferation of skin cells
- In psoriasis, there is an accelerated turnover of skin cells, leading to the rapid production and accumulation of new skin cells. This process is known as hyperproliferation
- The increased proliferation of skin cells is driven by the abnormal signaling of T-cells and the release of inflammatory cytokines, particularly TNF-alpha, IL-17, and IL-23. These cytokines stimulate the production of keratinocytes (the primary skin cells) and disrupt the normal balance between cell growth and shedding
Angiogenesis and increased blood flow
- Psoriasis is characterized by increased blood vessel formation (angiogenesis) in the affected skin areas. This process is stimulated by angiogenic factors released during the inflammatory response
- The increased blood flow contributes to the characteristic redness and warmth seen in psoriasis lesions
Abnormal differentiation and function of skin cells
- In psoriasis, the differentiation and function of skin cells, particularly keratinocytes, are altered
- The keratinocytes in psoriatic lesions differentiate more rapidly than normal, leading to the formation of thickened, scaly patches of skin
- Additionally, there is an abnormal production of keratin, resulting in the characteristic silvery-white scales seen in psoriasis
The complex interplay of these factors contributes to the development of psoriasis and its characteristic clinical features. The understanding of the pathophysiology of psoriasis has led to the development of targeted therapies aimed at specific components of the immune system and inflammatory pathways involved in the condition. However, further research is still needed to fully elucidate the intricacies of psoriasis pathophysiology.
What are the symptoms of psoriasis?
Psoriasis is a chronic skin condition that can manifest in various ways. The symptoms of psoriasis may vary in severity and presentation from person to person. Here are the common symptoms associated with psoriasis:
Plaque formation symptoms
Plaque psoriasis is the most common form of psoriasis and is characterized by the formation of raised, red patches called plaques. These plaques are typically covered with silvery-white scales and can vary in size and shape. They commonly appear on the elbows, knees, scalp, and lower back, but can occur on any part of the body
Itching and irritation symptoms
Psoriasis plaques often cause itching, irritation, and discomfort. Scratching the affected areas can worsen symptoms and lead to potential skin damage
Dry skin symptoms
Psoriasis-prone skin is typically dry and may exhibit a rough or cracked texture. The dryness can contribute to increased itching and discomfort
Scaling and flaking symptoms
The plaques of psoriasis can produce an excessive buildup of skin cells, resulting in the formation of silvery-white scales on the surface. These scales may flake off and be visible on clothing or bedding.
Redness and inflammation symptoms
Psoriasis lesions are characterized by redness and inflammation due to the underlying immune system response and increased blood flow to the affected areas. The skin may appear visibly inflamed and may feel warm to the touch
Nail change symptoms
Psoriasis can affect the nails, causing changes such as pitting (small depressions or indentations), discoloration, thickening, crumbling, or separation from the nail bed. Nail changes can occur alongside skin symptoms or independently
Joint pain and swelling symptoms
Some individuals with psoriasis may develop a related condition called psoriatic arthritis, which causes joint pain, swelling, stiffness, and reduced range of motion. Psoriatic arthritis can affect any joint, including those in the fingers, toes, wrists, knees, and ankles.
The severity of symptoms can range from mild to severe, and psoriasis symptoms may come and go in cycles of flare-ups and remission. The impact of psoriasis on an individual’s quality of life can vary depending on the extent of the condition and its effects on physical appearance, daily activities, and emotional well-being. Consulting with a healthcare professional, typically a dermatologist, is important for accurate diagnosis, personalized treatment, and management of psoriasis symptoms.
What are the complications of psoriasis?
Psoriasis is a chronic inflammatory condition that can have several complications, both related to the skin and other aspects of overall health. Here are some common complications associated with psoriasis:
Psoriatic arthritis
Psoriatic arthritis is a related condition that can occur in individuals with psoriasis. It causes inflammation, pain, and swelling in the joints, leading to stiffness and reduced range of motion. Psoriatic arthritis can affect any joint, including those in the fingers, toes, wrists, knees, and ankles. There is increasing evidence to suggest that people with psoriasis may be at higher risk for developing other health conditions, including liver disease
Skin infections
Due to the compromised skin barrier and chronic inflammation, individuals with psoriasis are more susceptible to skin infections. Bacterial infections (such as cellulitis or impetigo) and fungal infections (like candidiasis) can develop in psoriasis lesions
Koebner phenomenon
The Koebner phenomenon refers to the development of new psoriasis lesions in areas of skin injury or trauma. Skin trauma, such as cuts, burns, or scratches, can trigger the appearance of psoriatic lesions at the site of injury
Emotional and psychological impact
Psoriasis can significantly impact an individual’s emotional well-being and quality of life. The visible symptoms, such as red and scaly skin patches, can lead to self-consciousness, low self-esteem, anxiety, and depression. Social stigma and misconceptions about psoriasis can further contribute to psychological distress
Cardiovascular disease
Chronic inflammation associated with psoriasis is known to contribute to an increased risk of cardiovascular diseases, including heart attacks, strokes, and atherosclerosis (hardening of the arteries). Individuals with severe psoriasis or psoriatic arthritis may have a higher risk of developing cardiovascular complications
Metabolic syndrome
There is an association between psoriasis and metabolic syndrome, a cluster of conditions that includes obesity, high blood pressure, high blood sugar levels, and abnormal cholesterol levels. Metabolic syndrome increases the risk of heart disease, stroke, and type 2 diabetes
Other Autoimmune diseases
Individuals with psoriasis may have an increased risk of developing other autoimmune disorders, such as Crohn’s disease, rheumatoid arthritis, or systemic lupus erythematosus.
What are the management and treatment options for psoriasis?
The management and treatment of psoriasis aim to alleviate symptoms, reduce inflammation, slow down skin cell turnover, and improve overall quality of life. The approach to treatment may vary depending on the severity of symptoms, the extent of skin involvement, and individual preferences. Here are the main management and treatment options for psoriasis
Topical treatments
- Corticosteroids: Topical corticosteroids are commonly prescribed to reduce inflammation and relieve itching. They come in varying strengths and formulations
- Vitamin D analogues: Topical medications containing vitamin D derivatives, such as calcipotriene, help regulate skin cell growth and reduce scaling
- Topical retinoids: Retinoid creams or gels, derived from vitamin A, can help normalize skin cell production and reduce inflammation
- Topical calcineurin Inhibitors: Non-steroidal creams or ointments, such as tacrolimus or pimecrolimus, can be used for sensitive areas like the face and skin folds
Phototherapy
- Ultraviolet (UV) light therapy involves controlled exposure to UV light, either from natural sunlight or artificial light sources. It helps slow down skin cell turnover and reduce inflammation. Types of phototherapy include narrowband UVB, broad-spectrum UVB, and PUVA (psoralen plus ultraviolet A) therapy
Systemic medications
- For moderate to severe psoriasis, oral or injectable medications may be prescribed. These include:
- Methotrexate: An immunosuppressant that helps slow skin cell growth
- Cyclosporine: Suppresses the immune system and reduces inflammation
- Retinoids: Oral retinoids, such as acitretin, are used for severe cases
- Biologics: Targeted immune-modulating medications that block specific molecules involved in the immune response, such as TNF-alpha, IL-17, or IL-23
Oral medications
- Oral medications like apremilast, a phosphodiesterase-4 inhibitor, can be prescribed for moderate to severe psoriasis
Lifestyle modifications
- Regular moisturization to prevent dryness and scaling
- Avoiding triggers, such as stress, certain medications, or skin injuries
- Maintaining a healthy weight through a balanced diet and regular exercise
- Avoiding smoking and excessive alcohol consumption, as they can worsen symptoms
Supportive Therapies
- Emollients and moisturizers to keep the skin hydrated
- Salicylic acid or urea-based creams to reduce scaling
- Coal tar preparations to help slow down skin cell growth
- Supportive counseling or therapy to manage psychological effects
Biologics in the treatment of psoriasis
Biologics are a type of treatment for moderate to severe psoriasis that work by targeting specific parts of the immune system. They are typically used in patients who have not responded to other treatments, or in those with psoriatic arthritis. Here are some of the commonly used biologics in the treatment of psoriasis:
TNF-alpha inhibitors
These work by blocking the action of a substance in the body called tumor necrosis factor-alpha (TNF-alpha), which plays a role in systemic inflammation
- Etanercept (Enbrel)
- Infliximab (Remicade)
- Adalimumab (Humira)
- Certolizumab pegol (Cimzia)
Interleukin inhibitors
These work by blocking proteins in the immune system, called interleukins, that play a key role in inflammation and are believed to contribute to psoriasis.
- Ustekinumab (Stelara): Blocks interleukins 12 and 23
- Secukinumab (Cosentyx) and Ixekizumab (Taltz): Block interleukin 17-A
- Brodalumab (Siliq): Blocks the receptor for interleukin 17
- Risankizumab (Skyrizi) and Guselkumab (Tremfya): Block interleukin 23
T-cell inhibitors
These work by blocking the action of T cells, a type of white blood cell that plays a role in psoriasis.
- Abatacept (Orencia)
Phosphodiesterase-4 (PDE4) inhibitors
These work by blocking an enzyme called PDE4, which plays a role in inflammation
- Apremilast (Otezla)
All of these drugs are administered either through an injection or intravenous infusion. They are systemic medications, meaning they affect the entire body, not just the skin. Biologics are typically used when psoriasis is severe, does not respond to other treatments, or in the presence of psoriatic arthritis
Biologics can have side effects, which can include infections and injection site reactions.
What medications are used to manage or treat psoriasis?
Psoriasis treatment often involves the use of medications to help manage symptoms, reduce inflammation, and slow down the excessive skin cell growth associated with the condition. Here are some of the medications commonly used in the management and treatment of psoriasis
Topical medications
- Corticosteroids: These anti-inflammatory medications are available in various strengths and formulations (creams, ointments, lotions) to reduce itching, redness, and inflammation
- Vitamin D Analogues: These topical medications, such as calcipotriene or calcitriol, help regulate skin cell growth and reduce scaling and inflammation
- Topical Retinoids: Derived from vitamin A, retinoids like tazarotene can slow down skin cell growth and reduce inflammation
- Calcineurin Inhibitors: Topical calcineurin inhibitors, such as tacrolimus or pimecrolimus, can be used for sensitive areas like the face and skin folds to reduce inflammation
Phototherapy therapy
- Narrowband UVB Therapy: Controlled exposure to a specific wavelength of ultraviolet B (UVB) light helps slow down skin cell turnover and reduce inflammation
- PUVA Therapy: Psoralen, a light-sensitizing medication, is combined with exposure to ultraviolet A (UVA) light to slow down excessive cell growth
Systemic Medications
- Methotrexate: An oral or injectable medication that suppresses the immune system and reduces skin cell turnover
- Cyclosporine: An immunosuppressant that suppresses the immune system response and reduces inflammation
- Retinoids: Oral retinoids, such as acitretin, can be prescribed for severe cases to slow down skin cell growth
- Biologics: Targeted immune-modulating medications that block specific molecules involved in the immune response, such as tumor necrosis factor-alpha (TNF-alpha), interleukin-17 (IL-17), or interleukin-23 (IL-23). Biologics are usually administered via injections or infusions and require regular monitoring
Oral medication
Apremilast: A phosphodiesterase-4 inhibitor that helps regulate inflammation and immune responses
It’s important to note that medication choices may vary based on individual factors such as the severity of symptoms, overall health, response to treatment, and any underlying conditions. Treatment plans are often tailored to each person’s needs, and regular follow-up with healthcare professionals, typically dermatologists, is crucial for monitoring progress, adjusting medications, and ensuring optimal management of psoriasis.
What organizations support people living with psoriasis in the US?
- National Psoriasis Foundation (NPF) – A non-profit organization dedicated to driving efforts to cure psoriatic disease and improving the lives of those affected
- American Academy of Dermatology (AAD) – Provides extensive resources and guidelines for the treatment and management of psoriasis
- Psoriasis and Psoriatic Arthritis Alliance (PAPAA) – Based in the UK, but provides resources and information for people around the world, including the US
- Psoriasis Cure Now (PCN) – A nonprofit organization dedicated to raising awareness, advocating for research, and supporting patients
- Psoriasis Help Organisation – An online community with forums where patients can share experiences and advice
- Skin of Color Society (SOCS) – Promotes awareness of skin disease, including psoriasis, in people of color
- Arthritis Foundation – Provides resources and support for individuals dealing with psoriatic arthritis, a condition that can occur in conjunction with psoriasis
- International Federation of Psoriasis Associations (IFPA) – Offers resources, support, and advocacy for people affected by psoriasis and psoriatic arthritis
- American Chronic Pain Association (ACPA) – Offers resources for managing the chronic pain that can come with conditions like psoriatic arthritis
- Patient Advocate Foundation (PAF) – Provides support and assistance to patients with chronic and life-threatening diseases, including psoriasis. They offer case management services, financial aid, and other resources
What organizations support people living with psoriasis in the UK?
- Psoriasis Association – This organization offers extensive resources and support for people affected by psoriasis in the UK
- Psoriasis and Psoriatic Arthritis Alliance (PAPAA) – PAPAA provides a positive approach towards psoriasis and psoriatic arthritis in the UK
- British Association of Dermatologists (BAD) – While not solely dedicated to psoriasis, BAD provides resources and patient information leaflets on a wide range of skin conditions including psoriasis
- British Skin Foundation (BSF) – The BSF provides information and support for a range of skin conditions, including psoriasis. They also fund research into various skin conditions
- British Society for Rheumatology (BSR) – Provides resources and support for individuals dealing with psoriatic arthritis, a condition that can occur in conjunction with psoriasis
- Salford Royal NHS Foundation Trust – Salford’s Dermatology Centre is one of the largest investigative and treatment centres for skin disease in Europe and provides resources and treatments for psoriasis health conditions
- Guy’s and St Thomas’ NHS Foundation Trust – Provides the Psoriasis Shout Out, an initiative to raise awareness of psoriasis
- National Eczema Society – Although primarily focused on eczema, they also offer resources and support for those dealing with various skin conditions, including psoriasis
Summary
Psoriasis is a chronic skin condition that requires ongoing management and care. By understanding its symptoms, causes, and triggers, individuals can take steps to prevent flare-ups, manage symptoms effectively, and improve their quality of life. Treatment approaches range from topical medications to phototherapy, systemic medications, and lifestyle adjustments. It is important to work closely with healthcare professionals, such as dermatologists, to develop personalized treatment plans based on individual needs. With proper management and support, individuals with psoriasis can achieve symptom control and lead fulfilling lives.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
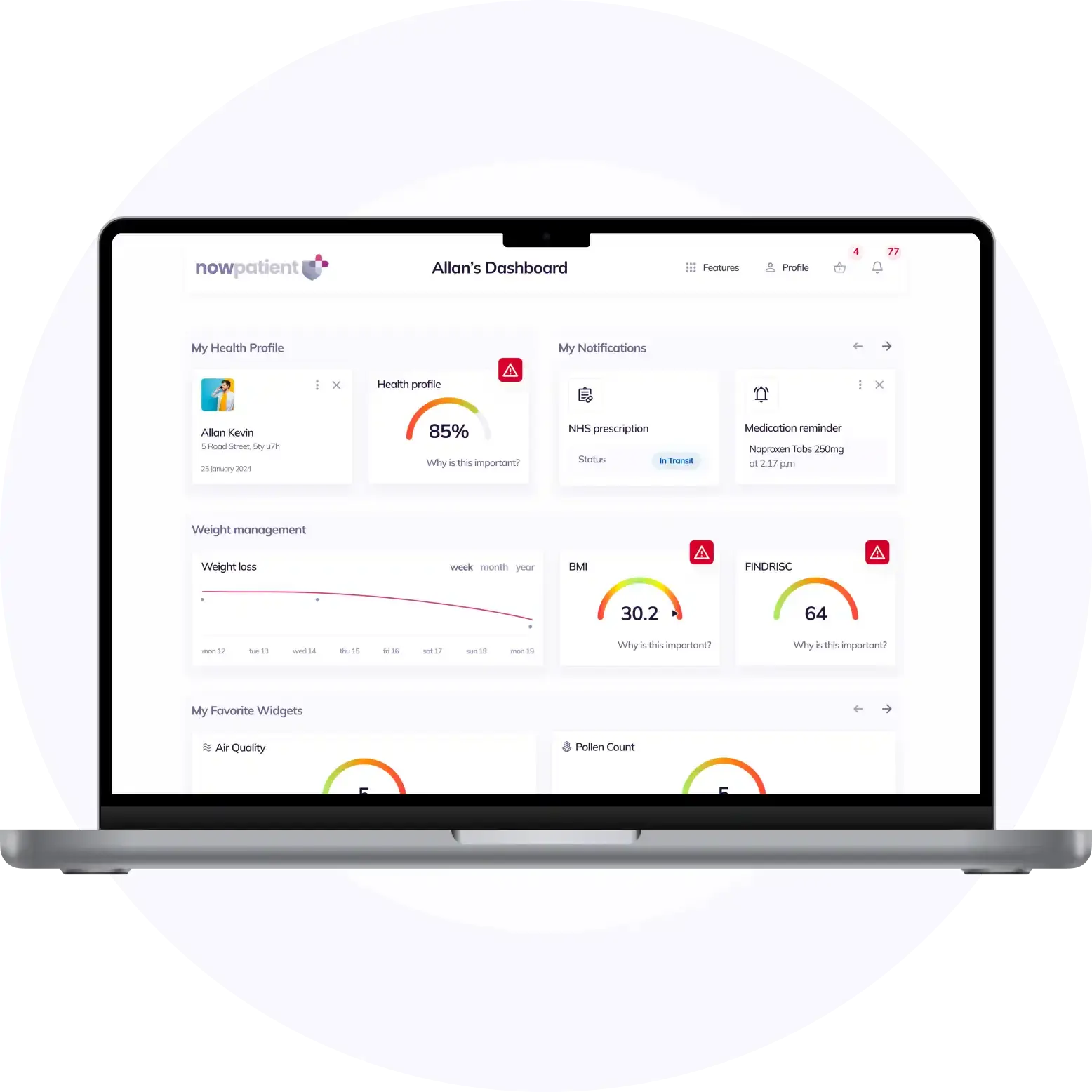
What is NowPatient
Telehealth and Online Pharmacy
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process