Primary Biliary Cirrhosis
Treatments & Medications
Is the cost of your Primary Biliary Cirrhosis medication too expensive or unaffordable?
You may qualify for programs where you can pay as little as $0 per fill, subject to income and insurance status.
This content is intended for US audiences only

Primary Biliary Cirrhosis (PBC), now known as Primary Biliary Cholangitis, is a chronic liver disease characterized by the progressive destruction of the bile ducts within the liver. These bile ducts play a crucial role in transporting bile, a fluid produced by the liver that aids in the digestion of fats. Without correctly functioning bile ducts, bile accumulates in the liver, eventually causing liver damage and cirrhosis of the liver.
This autoimmune disorder primarily affects women, typically between the ages of 45 to 65. While PBC may not always present noticeable symptoms in its early stages, it can have severe implications if left untreated.
The Pathophysiology of PBC: Unraveling the Immune system’s role
The exact cause of PBC remains unknown, but researchers believe it to be an autoimmune disease. In PBC, the immune system mistakenly attacks the small and medium-sized bile ducts, leading to their destruction. This immune-mediated destruction is thought to involve activated CD4 and CD8 lymphocytes. As a result, chronic cholestasis ensues, causing bile to accumulate within the liver and resulting in inflammation and scarring.
Studies have shown that individuals with PBC often have abnormalities in their immune system, including elevated levels of immunoglobulins, particularly immunoglobulin M (IgM). Additionally, the presence of antimitochondrial antibodies (AMAs) in serum is a hallmark of PBC, with a specificity of 98% for the disease. These AMAs can be detected in approximately 90-95% of PBC patients and are classified into four profiles (A, B, C, and D) depending on the specific antibodies present.
People with Primary Biliary Cholangitis may also be diagnosed with other autoimmune diseases, such as a endocrinological, rheumatological, gastrointestinal, dermatological, or pulmonary conditions, suggesting shared immune and genetic abnormalities. Common associations include hypothyroidism, Sjögren’s syndrome, rheumatoid arthritis, and coeliac disease.
Recognizing the symptoms: From fatigue to pruritus
In the early stages of PBC, many individuals remain asymptomatic, without any noticeable symptoms, making it challenging to diagnose. However, as the disease progresses, individuals may experience a range of symptoms. The most commonly reported symptom is fatigue, affecting approximately 65% of patients. Pruritus (itchy skin), is another prevalent symptom experienced by 55% of individuals with PBC. Other symptoms may include joint and muscle pain, swollen ankles or feet, upper right sided abdominal pain, and dry eyes and mouth (Sicca syndrome).
As the disease advances, physical examination findings may include hepatomegaly (enlarged liver), hyperpigmentation (darkening of the skin), splenomegaly (enlarged spleen), osteoporosis (brittle bones leading to fractures), high cholesterol, hypothyroidism (underactive thyroid), weight loss, yellowing of the skin and eyes (jaundice), steatorrhoea (diarrhea that may include greasy stools), and the presence of xanthomas and xanthelasmas (small yellow or white bumps under the skin or around the eyes). In advanced stages of PBC, individuals may exhibit stigmata of cirrhosis, such as spider nevi, palmar erythema, ascites (buildup of fluid in the abdomen), and muscle wasting.
Causes and risk factors
The exact cause of primary biliary cholangitis is still unknown. However, researchers believe that it is an autoimmune disease, where the body’s immune system attacks the body, with a combination of genetic and environmental factors contributing to its development. Women are at a higher risk of developing PBC, with a ratio of 10-to-1 compared to men. Additionally, there may be a familial predisposition to the disease, suggesting a genetic component.
Inflammation of the liver seen in primary biliary cholangitis begins when white blood cells called T cells (T lymphocytes), start to build up in the liver. Usually, these cells help to defend the body against invading bacteria and viruses. However, in primary biliary cholangitis, these T cells attack and destroy cells that line the small bile ducts in the liver.
Inflammation in the small bile ducts spreads, eventually damaging other cells in the liver. The cells that die, are replaced with scar tissue (fibrosis), leading to cirrhosis. The scarring of liver tissue in cirrhosis prevents your liver from work properly.
Diagnostic approaches: Unveiling the lab tests and imaging studies
Diagnosing primary biliary cholangitis typically involves a thorough evaluation of medical history, physical examination, and specific laboratory tests. Blood tests play a crucial role in the diagnosis, as they can detect elevated levels of certain enzymes and antibodies associated with PBC.
When PBC is suspected, various laboratory tests can aid in diagnosis. Significant elevations of alkaline phosphatase (ALP), γ-glutamyl transpeptidase (GGTP), and immunoglobulin levels, particularly IgM, are often observed in PBC patients. Aminotransferases such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST) may also be elevated. Additionally, abnormalities in lipid and cholesterol levels, erythrocyte sedimentation rate, bilirubin level, and prothrombin time can indicate disease progression to cirrhosis.
The presence of antimitochondrial antibodies (AMAs) in serum is a key diagnostic marker for PBC. While they are detected in the majority of patients, AMA-negative PBC can occur in some individuals. Imaging studies, including abdominal ultrasonography, CT scanning, and MRI’s may be used to assess the liver and rule out other conditions. These tests are crucial in evaluating liver and bile duct abnormalities, ruling out biliary obstruction, and monitoring disease progression. These imaging modalities can detect changes such as increased echogenicity of the liver parenchyma, portal lymphadenopathy, and signs of portal hypertension.
Managing PBC: Slowing disease progression and alleviating symptoms
While there is no cure for primary biliary cholangitis, various treatment options are available to manage the disease and slow its progression. The primary goal of PBC treatment is to preserve liver function, alleviate symptoms, and prevent complications. Ursodiol, a naturally occurring bile acid (ursodeoxycholic acid or UDCA), is the first-line medication used to slow the progression of the disease. It helps move bile out of the liver and into the small intestine, reducing liver inflammation. If Ursodiol is used early enough, it may improve liver function and prevent or delay the need for a liver transplant. Those with Primary Biliary Cholangitis (PBC) must take Ursodiol every day for the rest of their lives.
Obeticholic acid, either in combination with UDCA or as monotherapy, may be considered for patients who do not respond adequately to UDCA or cannot tolerate it. In addition to UDCA and obeticholic acid, other medications may be prescribed to manage specific symptoms and complications of primary biliary cholangitis. Pruritus, a common and often bothersome symptom, can be alleviated with antihistamines, cholestyramine, colestipol, rifampin, or dronabinol. Vitamin replacement therapy, including vitamins A, D, E, and K, may be necessary to address deficiencies caused by malabsorption. Calcium supplements may be added to help treat or prevent weak or soft bones (osteoporosis). Lifestyle changes such as maintaining a healthy diet, exercising regularly, and avoiding alcohol and smoking can also help manage PBC. It is essential to work closely with healthcare professionals to find the most effective treatment plan for individual needs.
Lifestyle changes and supportive care
In conjunction with medication, lifestyle changes and supportive care can play a significant role in managing primary biliary cholangitis. A healthy, well-balanced diet is crucial to support liver health and manage potential complications. It is recommended to avoid alcohol and maintain a diet low in saturated fats. Regular exercise, stress management techniques, and support from healthcare professionals and support groups can also be beneficial.
Regular monitoring and follow-up care are crucial for individuals with primary biliary cholangitis. This may involve regular blood tests to assess liver function, monitor medication effectiveness, and detect any potential complications. Imaging studies and liver biopsies may also be performed periodically to evaluate disease progression and assess the need for treatment adjustments.
Living with Primary Biliary Cholangitis: Tips and strategies
Living with primary biliary cholangitis can be challenging, but there are ways to manage the disease and improve quality of life. It is important to prioritize self-care, follow treatment plans, and maintain open communication with healthcare professionals. Engaging in a supportive community, practicing stress management techniques, and seeking emotional support can also be beneficial.
Potential complications: From osteoporosis to liver failure
If left untreated or poorly managed primary biliary cholangitis can lead to various complications in advanced stages. Osteoporosis, characterized by weak and brittle bones, is a common complication, particularly in late-stage PBC. Portal hypertension, which results from increased blood pressure in the portal veins, can lead to the development of ascites and varices. Malabsorption, malnutrition, vitamin deficiencies, and deficiencies in fat-soluble vitamins are also concerns in PBC patients.
As the liver function deteriorates, liver failure becomes a significant risk. Regular monitoring, early intervention, screening for liver cancer, and addressing complications such as encephalopathy and fluid and electrolyte imbalances are crucial in managing advanced PBC to prevent complications. In severe cases, liver transplantation may be necessary to improve long-term outcomes when medical treatment is no longer sufficient to control the disease.
Research and future directions
Ongoing research is essential for advancing the understanding and management of primary biliary cholangitis. Studies focus on identifying novel therapeutic approaches, improving diagnostic tools, and exploring potential genetic and environmental factors contributing to the disease. Participating in clinical trials may provide opportunities for individuals to access emerging treatments and contribute to scientific advancements.
Conclusion: Navigating life with PBC
Primary Biliary Cirrhosis, now known as Primary Biliary Cholangitis, is a chronic liver disease that primarily affects women. Although the exact cause remains unknown, it is believed to be an autoimmune disorder characterized by the destruction of bile ducts within the liver.
Early detection, proper management, lifestyle changes, and adherence to treatment can significantly slow disease progression and improve outcomes for individuals with PBC. By understanding the symptoms, staying informed, working closely with healthcare professionals, and adopting a proactive approach to self-care, and available treatment options, individuals with primary biliary cholangitis can lead fulfilling lives, while effectively managing the disease.
Sources
- Primary biliary cholangitis – Symptoms and causes – Mayo Clinic
- Primary Biliary Cholangitis: What It Is, Symptoms, Treatment
- Primary Biliary Cholangitis: Symptoms & Causes
- Primary Biliary Cholangitis (Primary Biliary Cirrhosis): Practice Essentials, Background, Pathophysiology
- Primary biliary cirrhosis – Better Health Channel
- Primary Biliary Cholangitis (Primary Biliary Cirrhosis) – NIDDK
- Primary biliary cholangitis – NHS
- Primary Biliary Cirrhosis – Symptoms and Causes
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
What is NowPatient
Telehealth and Online Pharmacy
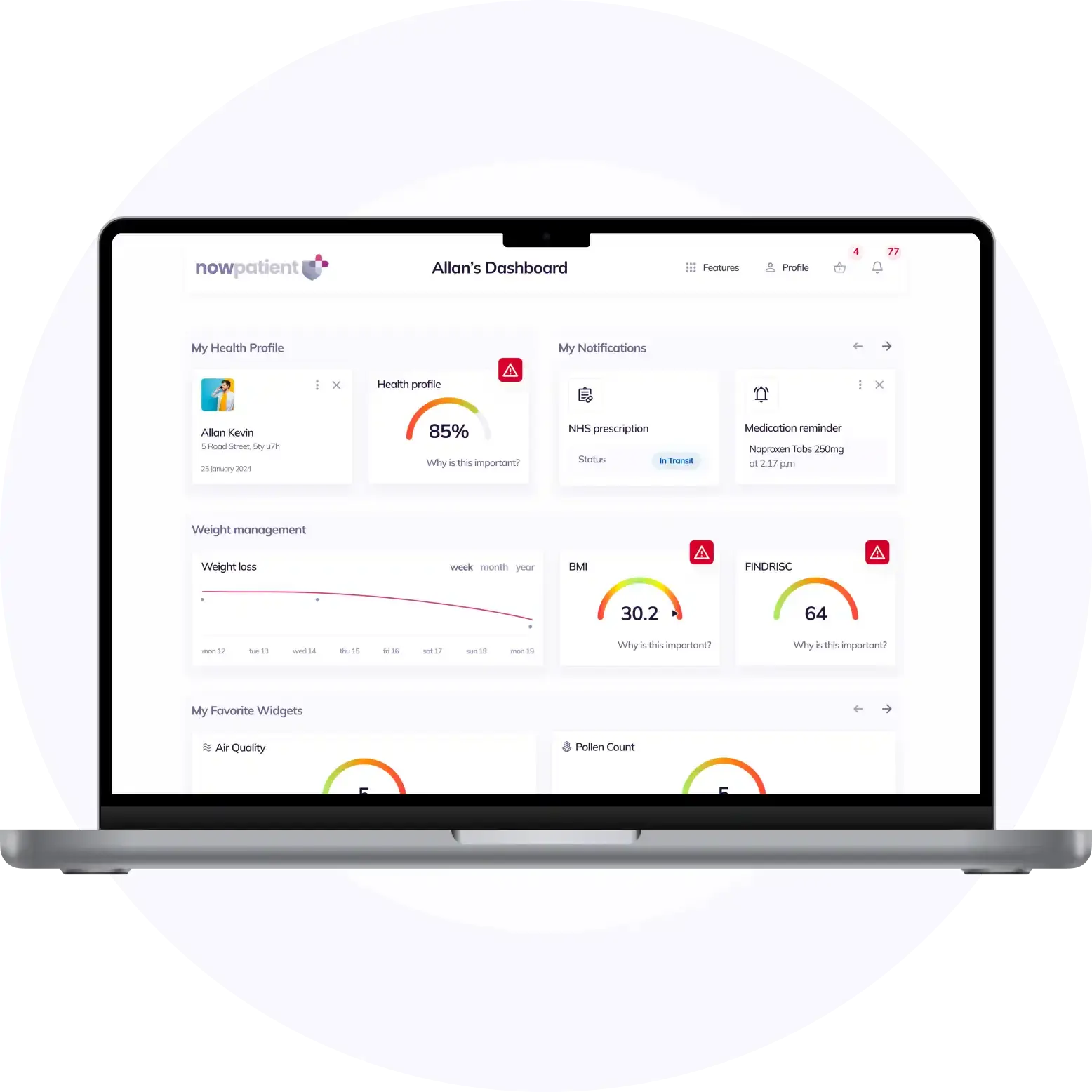
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process