Peripheral Arterial Disease
Treatments & Medications
Is the cost of your Peripheral Arterial Disease medication too expensive or unaffordable?
You may qualify for programs where you can pay as little as $0 per fill, subject to income and insurance status.
This content is intended for US audiences only

What is the definition of peripheral arterial disease?
Peripheral Arterial Disease (PAD), also known as peripheral vascular disease, is a circulatory disorder characterized by the narrowing or blockage of the arteries that supply blood to the extremities, most commonly the legs. It is a form of atherosclerosis, a condition where fatty deposits called plaques build up in the artery walls, leading to reduced blood flow to the affected areas. As a result, the muscles and tissues in the limbs do not receive an adequate supply of oxygen and nutrients, causing various symptoms and impairing overall limb function. PAD is a chronic condition that can progressively worsen if left untreated, potentially leading to complications such as non-healing wounds, infections, and even limb amputation. Proper diagnosis and management of PAD are essential to improve symptoms, prevent complications, and maintain a good quality of life for individuals affected by this condition.
What are the causes and risk factors associated with peripheral arterial disease?
Peripheral Arterial Disease (PAD) is primarily caused by atherosclerosis, a condition characterized by the accumulation of fatty deposits, known as plaques, in the walls of the arteries. These plaques narrow and harden the arteries, restricting blood flow to the limbs. Several factors contribute to the development of PAD and increase the risk of atherosclerosis:
Smoking
Cigarette smoking is one of the most significant risk factors for PAD. The chemicals in tobacco smoke damage blood vessels, promote inflammation, and accelerate the formation of plaques.
Diabetes
People with diabetes are at a higher risk of developing PAD. Elevated blood sugar levels can damage blood vessels, impairing their ability to dilate and affecting circulation.
Hypertension
Uncontrolled high blood pressure can lead to the hardening and narrowing of arteries, increasing the risk of atherosclerosis and PAD.
High Cholesterol
High levels of cholesterol, particularly low-density lipoprotein (LDL) cholesterol, contribute to the formation of plaques in the arteries. LDL cholesterol can accumulate in the arterial walls, leading to the narrowing of blood vessels.
Obesity
Excess body weight puts additional strain on the circulatory system and increases the risk of atherosclerosis and PAD.
Sedentary Lifestyle
Lack of regular physical activity weakens the circulatory system and contributes to the development of atherosclerosis. Engaging in regular exercise helps maintain healthy blood vessels and reduces the risk of PAD.
Age and Gender
The risk of PAD increases with age, particularly after the age of 50. Men are at a higher risk of developing PAD than women, although the gender gap narrows with advancing age.
Family History
Having a family history of PAD or atherosclerosis increases the likelihood of developing the condition. Genetic factors can influence the risk of developing atherosclerosis and PAD.
Other Medical Conditions
Certain medical conditions, such as chronic kidney disease, autoimmune diseases (e.g., lupus), and inflammatory conditions (e.g., rheumatoid arthritis), can increase the risk of PAD.
Ethnicity
Certain ethnic groups, such as African Americans, have a higher risk of developing PAD compared to other populations.
Other Risk Factors
Additional risk factors for PAD include a history of heart disease, stroke, or other cardiovascular conditions, as well as exposure to environmental toxins and pollutants.
It is important to note that the presence of these risk factors does not guarantee the development of PAD, but they increase the likelihood. Adopting a healthy lifestyle, managing chronic conditions, and minimizing risk factors can significantly reduce the risk of developing PAD and its complications.
What are the different types of peripheral arterial disease?
Peripheral Arterial Disease (PAD) encompasses various types depending on the location and extent of arterial involvement. The different types of PAD include:
Aortoiliac Disease
This type of PAD affects the large arteries in the abdomen and pelvis, known as the aorta and iliac arteries. Aortoiliac disease can cause pain, cramping, and fatigue in the lower back, hips, buttocks, and thighs.
Femoropopliteal Disease
Also called superficial femoral artery disease, this type of PAD involves the femoral artery and its branches in the thigh and knee region. Femoropopliteal disease can cause leg pain, cramping, and discomfort during walking or physical activity.
Tibial and Peroneal Artery Disease
This type of PAD affects the arteries in the lower leg, specifically the tibial and peroneal arteries. It can lead to pain, non-healing wounds, and ulcers in the feet and lower legs.
Multilevel Disease
Multilevel PAD involves multiple segments of the arterial system, affecting different areas such as the aorta, iliac, femoral, and lower leg arteries. It may involve a combination of aortoiliac, femoropopliteal, and tibial/peroneal disease. Multilevel PAD can cause widespread symptoms and may require comprehensive treatment approaches.
Critical Limb Ischemia (CLI)
Critical limb ischemia is an advanced stage of PAD characterized by severely reduced blood flow to the limbs. It is often associated with pain at rest, non-healing wounds, and tissue damage. CLI is the most severe form of PAD and requires immediate medical attention to prevent limb loss.
It’s important to note that these types of PAD can coexist or occur simultaneously in the same individual. The symptoms and severity of PAD can vary depending on the specific arteries involved and the extent of arterial blockage. Proper diagnosis, classification, and understanding of the specific type of PAD help guide treatment decisions and improve outcomes for individuals with the condition.
What is the pathophysiology of peripheral arterial disease?
The pathophysiology of Peripheral Arterial Disease (PAD) is primarily characterized by the development of atherosclerosis, a condition where fatty deposits, known as plaques, accumulate within the walls of the arteries. The following are the key steps involved in the pathophysiology of PAD
Endothelial Dysfunction
The inner lining of the arteries, called the endothelium, plays a crucial role in maintaining the health and function of blood vessels. Various factors, such as smoking, high blood pressure, and high cholesterol levels, can cause damage to the endothelial cells, leading to endothelial dysfunction. This dysfunction disrupts the normal regulation of blood vessel tone, inflammation, and clotting.
Lipid Accumulation and Inflammation
In response to endothelial dysfunction, lipids, particularly low-density lipoprotein (LDL) cholesterol, accumulate in the arterial wall. These lipids undergo oxidation, triggering an inflammatory response. Inflammatory cells, such as macrophages, migrate to the site and engulf the oxidized LDL, forming foam cells within the arterial wall.
Formation of Plaques
The accumulation of foam cells, along with smooth muscle cells and connective tissue, forms plaques within the arterial wall. Plaques are characterized by a fatty core covered by a fibrous cap.
Arterial Narrowing and Stenosis
As the plaques grow, they protrude into the lumen of the artery, narrowing the blood vessel and impeding blood flow. The narrowing of the artery reduces the supply of oxygen and nutrients to the tissues downstream.
Arterial Occlusion and Ischemia
In advanced cases, the plaques can rupture or become ulcerated, leading to the formation of blood clots. These clots can partially or completely block the artery, resulting in arterial occlusion. The occlusion further restricts blood flow, causing ischemia (lack of oxygen) in the affected tissues.
Collateral Circulation
Over time, in response to chronic arterial occlusion, the body attempts to establish collateral circulation, creating new blood vessels to bypass the blocked arteries. However, collateral vessels may not provide sufficient blood supply to meet the metabolic demands of the affected tissues.
Ischemic Tissue Damage
The reduced blood flow and oxygen supply result in tissue ischemia and damage. Persistent ischemia can lead to the development of non-healing wounds, ulcers, and tissue necrosis.
The pathophysiology of PAD involves a complex interplay of endothelial dysfunction, lipid accumulation, inflammation, plaque formation, arterial narrowing, and occlusion. The resulting reduction in blood flow and oxygen supply can lead to the characteristic symptoms of PAD, including leg pain, ulcers, and impaired tissue healing. Understanding the underlying pathophysiological processes helps guide the diagnosis, treatment, and management of PAD.
What are the signs and symptoms of peripheral arterial disease?
Peripheral Arterial Disease (PAD) can cause various signs and symptoms that primarily affect the lower extremities. The following are common signs and symptoms associated with PAD
Intermittent Claudication
This is the most characteristic symptom of PAD. Intermittent claudication refers to pain, cramping, or aching in the legs that occurs during physical activity, such as walking or climbing stairs. The pain typically subsides with rest and returns when activity resumes. The location of the pain depends on the location of the arterial blockage.
Pain at Rest
In advanced stages of PAD, when blood flow is severely restricted, individuals may experience pain even at rest, particularly at night when lying down. The pain is often described as aching, throbbing, or burning and may disrupt sleep.
Non-Healing Wounds or Ulcers
Reduced blood flow to the extremities can impair the healing process. Individuals with PAD may develop non-healing wounds or ulcers on the legs or feet, especially in areas that are frequently exposed to pressure or trauma.
Coldness or Decreased Temperature
The affected limbs may feel cold to the touch, and the skin may appear pale or bluish in color due to reduced blood flow and oxygen supply.
Changes in Skin Texture
The skin of the affected limbs may become dry, thin, and shiny. Hair loss may occur on the legs, and the nails may become brittle.
Weak or Absent Pulses
Healthcare providers may detect weak or absent pulses in the affected limbs during a physical examination. This finding suggests reduced arterial blood flow to those areas.
Erectile Dysfunction
In men, PAD can affect blood flow to the penile arteries, leading to erectile dysfunction.
It’s important to note that not everyone with PAD experiences symptoms. Some individuals may have asymptomatic PAD, especially in the early stages. However, the absence of symptoms does not mean the absence of the disease. Therefore, it’s crucial to be aware of the risk factors for PAD and seek medical evaluation if any concerning signs or symptoms are present. Early detection and appropriate management can help prevent complications and improve outcomes for individuals with PAD.
What are the stages of peripheral arterial disease (UK)?
In the United Kingdom, Peripheral Arterial Disease (PAD) is often classified into four stages based on the severity of symptoms and the degree of arterial obstruction. These stages are known as the Fontaine classification or the Rutherford classification. The stages are as follows
Stage I: Asymptomatic PAD
- In this stage, individuals with PAD do not experience any noticeable symptoms
- The arterial obstruction is present, but it does not cause significant symptoms or impair the individual’s daily activities
Stage II: Mild Claudication
- Individuals with Stage II PAD experience intermittent claudication, which is pain, cramping, or fatigue in the legs during physical activity, typically walking
- The pain is predictable and reproducible, occurring after a consistent distance of walking or a specific duration of exercise
- The symptoms resolve with rest
Stage III: Moderate Claudication
- Stage III PAD is characterized by more frequent and severe intermittent claudication symptoms
- The pain occurs with less activity and may limit daily activities, such as walking shorter distances or climbing fewer stairs
- Rest is required for symptom relief
Stage IV: Critical Limb Ischemia (CLI)
- This is the most severe stage of PAD
- Individuals with Stage IV PAD experience chronic, non-healing wounds or ulcers on the legs or feet
- Pain may be present even at rest and can be severe
- The affected limb may exhibit signs of ischemia, such as pallor, coolness, decreased sensation, and muscle weakness
- In advanced cases, tissue loss or gangrene may develop, putting the limb at risk of amputation
What are the stages of peripheral arterial disease (US)?
In the United States, the stages of peripheral arterial disease (PAD) are typically classified using the Fontaine classification or the Rutherford classification. These classifications categorize PAD based on the severity of symptoms and the extent of arterial blockage. The stages of PAD in the US are as follows:
Stage 0: Asymptomatic
- In this stage, individuals with PAD do not experience any symptoms
- Arterial blockage is present, but it does not cause noticeable symptoms or limitations in daily activities
Stage I: Mild Intermittent Claudication
- Individuals with Stage I PAD experience mild intermittent claudication, which is pain, cramping, or fatigue in the legs during physical activity
- The symptoms are typically relieved with rest
- The distance of walking or time of exercise required to elicit symptoms may vary
Stage II: Moderate Intermittent Claudication
- Stage II PAD is characterized by more frequent and severe intermittent claudication symptoms
- The pain occurs with a shorter distance of walking or a shorter duration of exercise compared to Stage I
- Rest is required for symptom relief
Stage III: Severe Intermittent Claudication
- Individuals with Stage III PAD experience severe intermittent claudication symptoms
- Pain or discomfort occurs even with minimal physical activity
- The pain may limit daily activities and quality of life
- Rest is required for symptom relief
Stage IV: Rest Pain
- Stage IV PAD is characterized by pain or discomfort in the feet or toes even at rest
- The pain may be severe and worsen at night
- Elevating the legs may provide temporary relief
- Ulcers or wounds may develop in the affected areas, indicating advanced disease
Stage V: Minor Tissue Loss
- Individuals in Stage V PAD have non-healing wounds or ulcers on the toes or feet
- The ulcers may be deep, exposing tendons or bones
- The risk of infection and complications is high
Stage VI: Major Tissue Loss or Gangrene
- Stage VI PAD represents the most severe form of the disease
- Individuals in this stage have extensive tissue loss, gangrene, or ulcers that involve a significant portion of the foot or leg
- The risk of amputation is high
How is peripheral arterial disease diagnosed?
Peripheral Arterial Disease (PAD) can be diagnosed through a combination of medical history assessment, physical examination, and diagnostic tests. The following methods are commonly used to diagnose PAD
Medical History
The healthcare provider or cardiology specialist will gather information about your symptoms, risk factors, and medical history. Details about your lifestyle, exercise habits, smoking history, and any existing medical conditions will be important in evaluating your risk for PAD.
Physical Examination
The healthcare provider will perform a thorough physical examination, including checking for pulses in various locations of the body, particularly in the legs and feet. They may also assess the temperature, color, and skin condition of the limbs.
Ankle-Brachial Index (ABI)
The ABI is a non-invasive test that compares the blood pressure in the ankles to that in the arms. The ratio between the two provides an estimation of blood flow in the lower extremities. A lower ABI value suggests reduced blood flow and may indicate the presence of PAD. This test is commonly used as a screening tool for PAD.
Doppler Ultrasound
Doppler ultrasound is an imaging technique that uses sound waves to assess blood flow through the arteries. It can help identify areas of arterial narrowing, obstruction, or blood flow abnormalities.
Segmental Pressure Measurements
In this test, blood pressure measurements are taken at various segments of the legs, including the thigh, calf, and ankle. Comparing the pressures in different segments helps identify the location and severity of arterial blockages.
Imaging Tests
Additional imaging tests may be ordered to visualize the arteries and evaluate the extent of arterial disease. These tests may include:
- Magnetic Resonance Angiography (MRA): This imaging technique uses magnetic fields and radio waves to create detailed images of blood vessels
- Computed Tomography Angiography (CTA): A specialized CT scan that provides detailed images of the blood vessels after injecting a contrast dye
- Digital Subtraction Angiography (DSA): This invasive procedure involves injecting a contrast dye into the arteries to visualize blood flow using X-rays
It’s important to note that the specific diagnostic tests used may vary depending on the individual’s symptoms, risk factors, and the healthcare provider’s preference.
What are treatment and management options for peripheral arterial disease?
The treatment and management of Peripheral Arterial Disease (PAD) aim to alleviate symptoms, improve blood flow, and reduce the risk of complications such as Coronary Artery Disease. The specific treatment approach depends on the severity of the disease, the presence of symptoms, and individual patient factors. The following are common treatment and management options for PAD
Lifestyle Modifications
- Smoking Cessation: Quitting smoking is crucial as it significantly reduces the progression of PAD
- Regular Exercise: Engaging in supervised exercise programs, such as walking or supervised treadmill exercise, can improve symptoms, increase walking distance, and promote collateral circulation
- Healthy Diet: Adopting a balanced diet that is low in saturated fats, blood cholesterol, and sodium can help manage PAD risk factors
Medications
- Antiplatelet Agents: Medications such as aspirin or clopidogrel are often prescribed to reduce the risk of blood clots and improve blood flow
- Cholesterol-Lowering Medications: Statins are commonly used to lower LDL cholesterol levels and slow the progression of atherosclerosis
- Blood Pressure Control: Medications to manage hypertension and maintain blood pressure within a healthy range may be prescribed
Interventional Procedures
- Angioplasty and Stenting: In this minimally invasive procedure, a balloon-tipped catheter is used to open narrowed or blocked arteries. A stent may be placed to keep the artery open
- Atherectomy: This procedure involves removing or cutting away plaque from the artery using specialized devices
Surgical Interventions
- Bypass Surgery: In severe cases of PAD, bypass surgery may be performed to reroute blood flow around blocked arteries, improving blood supply to the affected limb
- Amputation: In cases of advanced PAD with non-healing wounds, severe infection, or gangrene, amputation of the affected limb may be necessary to prevent life-threatening complications
Wound Care
Individuals with PAD and non-healing wounds or ulcers require careful wound care management. This may involve cleaning the wound, applying appropriate dressings, and addressing underlying circulation issues.
Medications for Symptom Relief
Medications such as cilostazol may be prescribed to improve walking distance and reduce symptoms of intermittent claudication.
Diabetes and Blood Sugar Control
Individuals with diabetes and PAD need to carefully manage their blood sugar levels to reduce the risk of complications and optimize overall health.
Risk Factor Management
Aggressive management of risk factors such as high blood pressure, high cholesterol levels, and diabetes is essential to prevent the progression of PAD and reduce the risk of complications.
Regular Follow-up and Monitoring
Regular check-ups and monitoring of PAD, including periodic imaging studies and assessments of symptoms, are crucial to evaluate the effectiveness of treatment and make necessary adjustments.
The specific treatment approach is individualized based on the patient’s condition and overall health. A comprehensive approach, including lifestyle modifications, medications, and interventions, can help manage PAD effectively and improve quality of life. It’s important to consult with a healthcare professional for an accurate diagnosis and to develop a personalized treatment plan.
What medications are used in peripheral arterial disease?
Antiplatelet Agents
- Aspirin
- Clopidogrel (Plavix)
- Ticagrelor (Brilinta)
- Cilostazol (Pletal): This medication also has vasodilatory effects.
Statins
- Atorvastatin (Lipitor)
- Simvastatin (Zocor)
- Rosuvastatin (Crestor)
- Pravastatin (Pravachol)
ACE inhibitors or ARBs (Angiotensin-Converting Enzyme Inhibitors or Angiotensin Receptor Blockers)
- Ramipril (Altace)
- Lisinopril (Prinivil, Zestril)
- Losartan (Cozaar)
- Valsartan (Diovan)
Beta-Blockers
- Metoprolol (Lopressor, Toprol XL)
- Carvedilol (Coreg)
- Bisoprolol (Zebeta)
Vasodilators
- Cilostazol (Pletal): This medication has both antiplatelet and vasodilatory effects
- Pentoxifylline (Trental): This medication can improve blood flow by reducing blood viscosity
Anticoagulants
- Warfarin (Coumadin)
- Rivaroxaban (Xarelto)
Symptom-Relief Medications
- Pain relievers (e.g., acetaminophen, nonsteroidal anti-inflammatory drugs)
- Medications for managing intermittent claudication symptoms
What are the complications of peripheral arterial disease?
Peripheral Arterial Disease (PAD) can lead to various complications, particularly if left untreated or poorly managed. The reduced blood flow to the extremities can result in the following complications
Non-Healing Wounds and Ulcers
The inadequate blood supply to the affected limbs impairs the healing process. Even minor injuries or wounds may not heal properly, leading to the development of non-healing wounds and ulcers, particularly on the feet and lower legs. These ulcers can become chronic and may increase the risk of infection.
Infections
Reduced blood flow and compromised immune function in the affected limbs increase the susceptibility to infections. Non-healing wounds, ulcers, or foot injuries can become infected, and the infection may spread to the surrounding tissues, leading to cellulitis or deep tissue infections.
Gangrene
In severe cases of PAD, where blood flow to the limbs is severely compromised, tissue death or gangrene can occur. Gangrene is characterized by the death of body tissues due to a lack of oxygen and nutrients. It may result in severe pain, foul-smelling wounds, and black or discolored skin. Gangrene is a serious complication that may necessitate urgent medical intervention, including amputation of the affected limb to prevent the spread of infection.
Amputation
If the complications of PAD, such as non-healing wounds, severe infections, or gangrene, cannot be effectively managed or treated, amputation of the affected limb may be necessary. Amputation is typically considered a last resort to prevent life-threatening complications and improve overall quality of life.
Cardiovascular Events
Individuals with PAD have a significantly increased risk of cardiovascular events, such as heart attack or stroke. The underlying atherosclerosis that causes PAD often affects multiple arterial beds, including the coronary arteries supplying the heart and the carotid arteries supplying the brain. The presence of PAD indicates a systemic vascular disease, and individuals with PAD are at a higher risk of developing cardiovascular complications.
Impaired Quality of Life
PAD can significantly impact an individual’s quality of life. The symptoms of intermittent claudication, pain, and limited mobility can restrict daily activities and reduce independence. Non-healing wounds, infections, and the need for ongoing medical care can also affect psychological well-being and overall quality of life.
Promising research and future direction of peripheral arterial disease
Promising research in the field of peripheral arterial disease (PAD) is focused on improving diagnostic techniques, understanding disease mechanisms, and exploring innovative treatment options. Some areas of research and future directions include
- Novel Diagnostic Approaches: Researchers are investigating new diagnostic methods and imaging techniques to improve the accuracy and early detection of PAD. This includes the development of advanced imaging technologies, such as magnetic resonance angiography (MRA) and computed tomography angiography (CTA), which provide detailed visualization of arterial structures and blood flow
- Biomarkers and Genetic Studies: Research is underway to identify specific biomarkers or genetic factors associated with PAD. Identifying these markers can aid in early detection, risk stratification, and personalized treatment approaches
- Pharmacological Interventions: Studies are exploring novel pharmacological agents to target the underlying mechanisms of PAD. This includes investigating medications that can promote angiogenesis (formation of new blood vessels), reduce inflammation, improve vascular function, and inhibit plaque formation
- Stem Cell Therapy: Researchers are investigating the use of stem cells to promote angiogenesis and tissue regeneration in individuals with PAD. Stem cell therapy holds potential for improving blood flow and promoting healing in non-healing wounds and ulcers
- Gene Therapy: Gene therapy research aims to use targeted gene delivery to stimulate the growth of new blood vessels and improve blood flow in individuals with PAD. By manipulating specific genes involved in angiogenesis, researchers hope to promote tissue repair and regeneration
- Exercise Rehabilitation Programs: Research is exploring the effectiveness of structured exercise rehabilitation programs in improving walking distance, reducing symptoms, and enhancing overall functional capacity in individuals with PAD. These programs aim to optimize exercise prescription, duration, and intensity to achieve the best outcomes for patients
- Telemedicine and Digital Health: The integration of telemedicine and digital health technologies has the potential to enhance access to healthcare for individuals with PAD. Remote monitoring, tele-consultations, and mobile applications can facilitate regular follow-up, medication adherence, and lifestyle modifications, leading to improved management and outcomes
- Patient Education and Self-Management: Educating individuals with PAD about their condition, risk factors, and self-management strategies is essential. Empowering patients with knowledge and resources can help them actively participate in their care, adhere to treatment plans, and make lifestyle changes necessary for better outcomes
What peripheral arterial disease support organisations are there available to support me in the UK?
- Circulation Foundation: The Circulation Foundation is a UK charity organization that focuses on raising awareness and supporting individuals with circulatory conditions, including PAD. They provide information resources, educational materials, and support for individuals and healthcare professionals
- British Heart Foundation (BHF): The British Heart Foundation is the largest heart charity in the UK and supports individuals with various cardiovascular conditions, including PAD. They offer information resources, helplines, support groups, and fundraising activities. Their website provides guidance on managing PAD and living a heart-healthy lifestyle
- Diabetes UK: Diabetes UK is a charity organization that supports individuals with diabetes, a condition that can increase the risk of PAD. They provide information resources, educational materials, and support for individuals living with diabetes and its associated complications, including PAD
- Leg Club Foundation: The Leg Club Foundation is a UK charity that focuses on promoting the holistic care of leg and foot conditions, including those related to PAD. They provide support groups, information resources, and access to professional advice and guidance
- Stroke Association: The Stroke Association is a charity organization that supports individuals affected by stroke. Stroke is a condition that can be related to PAD. They offer information resources, helplines, and support for individuals and families affected by stroke, including those with underlying PAD
What peripheral arterial disease support organisations are there available to support me in the US?
- Vascular Cures: Vascular Cures is a nonprofit organization dedicated to advancing research and improving vascular health. They provide resources, educational materials, and support for individuals with various vascular conditions, including PAD. They also fund research initiatives and promote awareness of vascular diseases
- Society for Vascular Surgery (SVS): The Society for Vascular Surgery is a professional medical society that focuses on vascular health. They provide educational resources, patient information, and access to vascular specialists through their website. They also support research and advocate for advancements in vascular care
- American Heart Association (AHA): The American Heart Association is a national organization that supports individuals with cardiovascular conditions, including PAD. They offer educational resources, information on risk factors and prevention, and access to support networks through local chapters and online communities
- PAD Coalition: The PAD Coalition is a collaborative network of organizations and healthcare professionals dedicated to promoting awareness, prevention, and treatment of PAD. They provide educational resources, patient advocacy, and support for individuals with PAD and their caregivers
- National Heart, Lung, and Blood Institute (NHLBI): The NHLBI is a government agency that provides resources and information on various cardiovascular conditions, including PAD. They offer educational materials, clinical guidelines, and research updates related to vascular health
Summary
Peripheral Arterial Disease is a common circulatory condition that can significantly impact an individual’s quality of life and increase the risk of serious complications. Early detection, proper diagnosis, and timely treatment are essential for managing symptoms, improving blood flow, and reducing the risk of complications. Lifestyle modifications, medication management, and interventional procedures play crucial roles in the comprehensive management of PAD. Ongoing research efforts continue to explore new avenues for diagnosis, treatment, and preventive strategies, offering hope for improved outcomes and enhanced quality of life for individuals affected by peripheral arterial disease.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
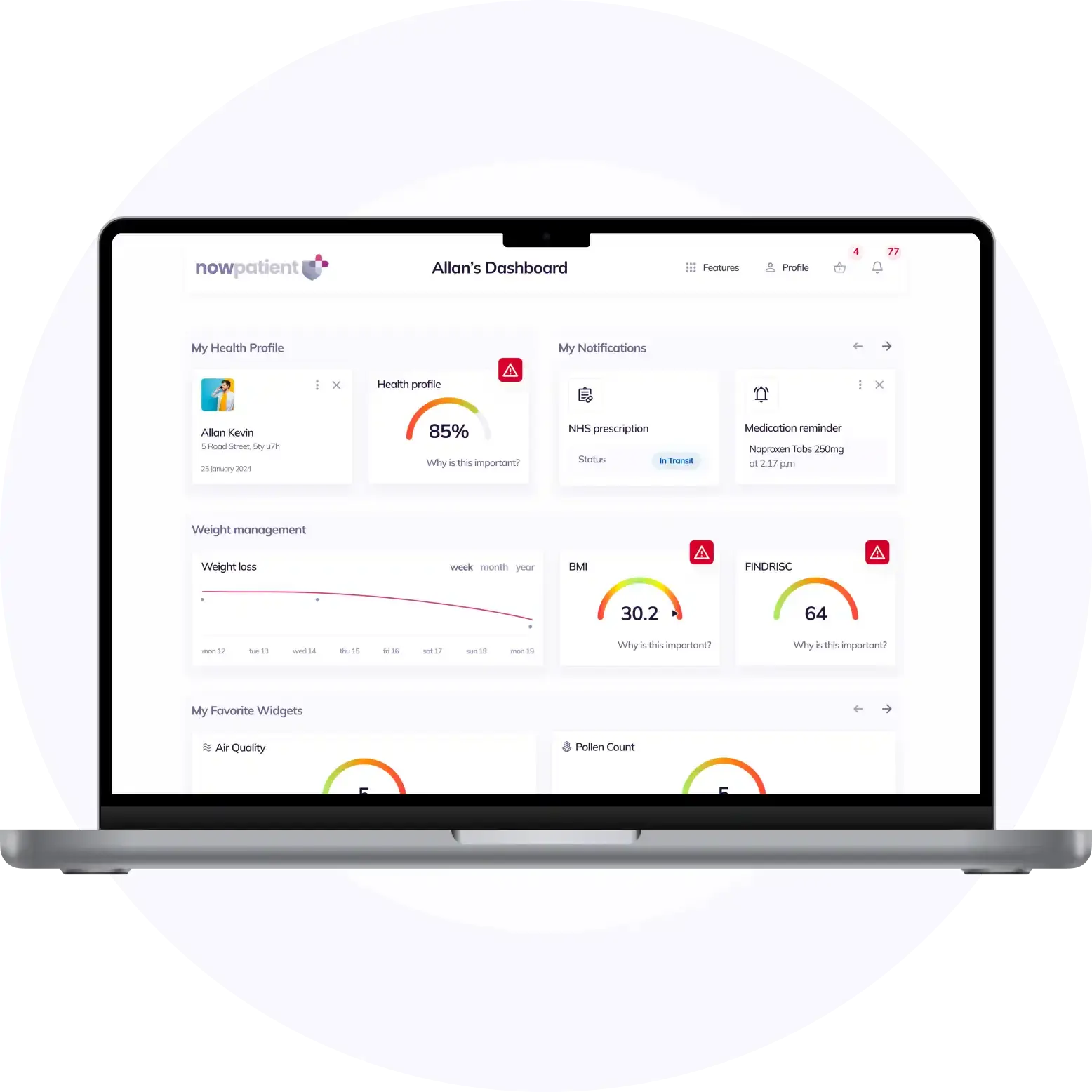
What is NowPatient
Telehealth and Online Pharmacy
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process