Opioid Dependence
Treatments & Medications
Is the cost of your Opioid Dependence medication too expensive or unaffordable?
You may qualify for programs where you can pay as little as $0 per fill, subject to income and insurance status.
This content is intended for US audiences only

Opioid dependence is a serious medical condition characterised by a compulsive and uncontrollable reliance on opioids. It poses significant challenges to public health globally. Here, we provide you with a comprehensive overview of opioid dependence, including its causes, symptoms, diagnostic criteria, and treatment approaches. Understanding the underlying mechanisms, identifying at-risk individuals, and implementing evidence-based interventions are essential for healthcare professionals to effectively manage opioid dependence and promote successful recovery.
What is the difference between opioid and opiates?
Some individuals differentiate between Opioids and Opiates as categories of narcotic drugs, while others use the terms interchangeably.
The main difference between an opiate and an opioid lies in their origin and composition:
- Opiates are a specific subset of narcotic drugs that are naturally derived from the opium poppy plant (Papaver somniferum). Opiates include compounds such as morphine, codeine, and the illicit drug heroin. Opiates are directly extracted or refined from the plant’s components, primarily the sap and fibers
- Opioids, on the other hand, encompass a broader category of narcotic drugs that include both natural and synthetic substances. While some opioid drugs may be derived from opium, many others are entirely synthetic and not sourced from natural plant matter. Opioids are typically produced in laboratories through chemical synthesis. Examples of opioids include drugs like oxycodone, hydrocodone, fentanyl, and methadone
Opiates and opioids are both classified as “narcotics.” The term “narcotic” simply refers to substances that induce sleepiness or numbness (derived from the Medieval Latin narcoticus, from the Greek narkoun, meaning “to benumb”).
What is the definition of opioid dependence?
Opioid dependence, also known as opioid use disorder (OUD), is a chronic medical condition characterized by a compulsive and uncontrollable reliance on opioids. Opioids are a class of drugs that include prescription pain relief medications like oxycodone, hydrocodone, fentanyl and morphine, as well as illicit substances such as heroin. Opioid medications are used, as pain relievers, in a clinical setting to treat moderate to severe pain.
In opioid dependence, individuals develop a physical and psychological reliance on opioids, leading to a range of problematic behaviours and consequences. They experience a strong urge to use opioids despite negative physical, psychological, and social effects. Opioid dependence involves changes in brain chemistry and reward pathways, contributing to the compulsive use and difficulty in stopping or reducing opioid intake.
What are the causes and risk factors of opioid dependence?
The development of opioid addiction is influenced by a combination of genetic, environmental, and individual factors. While the exact causes of opioid dependence are complex and multifaceted, several common factors contribute to its development. Here are the main causes and risk factors associated with opioid dependence
Genetics
- Genetic Predisposition: Certain genetic variations can increase an individual’s susceptibility to developing opioid dependence
- Family History: Having a family history of substance use disorders, including opioid dependence, can elevate the risk of developing the condition
Environmental Factors
- Access to Opioids: Easy access to prescription opioids, either through personal prescriptions or diversion, can contribute to opioid dependence
- Social and Peer Influence: Peer pressure, social norms, and exposure to individuals who misuse opioids can influence an individual’s initiation and continued use of opioids
- Exposure to Trauma: Experiencing physical, emotional, or sexual trauma, including adverse childhood experiences (ACEs), can increase the vulnerability to opioid dependence
- Socioeconomic Factors: Poverty, unemployment, and limited access to education and healthcare services are associated with a higher risk of opioid dependence
Pain Management
- Opioid Pain Medications: Long-term use of prescription opioids for the management of chronic pain can increase the risk of opioid dependence
- Inadequate Pain Management Alternatives: Limited access to non-opioid pain management strategies or lack of awareness regarding their efficacy can lead to over-reliance on opioids
Co-occurring Mental Health Disorders
- Individuals with mental health or psychiatry disorders, such as depression, anxiety, post-traumatic stress disorder (PTSD), or attention-deficit/hyperactivity disorder (ADHD), have an increased susceptibility to opioid dependence
- Self-Medication: Some individuals with mental health disorders may misuse opioids as a means of self-medication to alleviate emotional or psychological distress
Biological and Neurochemical Factors
- Neuroadaptation: Prolonged opioid use alters brain chemistry leading to tolerance, dependence, and cravings
- Opioid Receptor Genetics: Genetic variations in opioid receptors may influence an individual’s response to opioids and their susceptibility to dependence
6. Previous Substance Use
Individuals who have a history of substance use disorders, including alcohol or other drug dependencies, are at a higher risk of developing opioid dependence.
It’s important to note that while these factors contribute to the development of opioid dependence, not everyone with these risk factors will develop the condition. Individual experiences and circumstances can vary. Seeking professional help, early intervention, and implementing preventive measures are crucial in addressing opioid dependence and promoting optimal health outcomes.
What are the symptoms and clinical presentation of opioid dependence?
Here are the common symptoms and clinical presentations of opioid dependency
Craving and Urges
- An intense desire or compulsion to use opioids
- Persistent thoughts and preoccupation with obtaining and using opioids
Physical Dependence
- Developing tolerance to opioids, requiring higher doses to achieve the desired effect
- Experiencing opioid withdrawal symptoms when attempting to reduce or stop opioid use. Withdrawal symptoms may include nausea, vomiting, diarrhoea, muscle aches, sweating, insomnia, and anxiety
Impaired Control
- Difficulty controlling or limiting opioid use
- Unsuccessful attempts to cut down or quit opioid use
Neglecting Obligations
- Neglecting or reducing participation in important social, occupational, or recreational activities due to opioid use
- Failing to meet obligations at work, school, or home due to opioid use
Continued Use Despite Consequences
Continued use of opioids despite experiencing negative consequences, such as deteriorating physical health, strained relationships, financial difficulties, or legal problems.
Social and Behavioural Changes
- Withdrawal from social activities or previously enjoyed hobbies
- Increased isolation and spending significant time obtaining, using, or recovering from opioid use
- Engaging in deceptive behaviours to acquire opioids, such as llicit drug-seeking activities
Physical Health Issues
Opioid use can lead to a range of physical health problems, including respiratory depression, constipation, hormonal imbalances, increased risk of infectious diseases, and overdose. The majority of overdose deaths involve opioids.
Psychological and Emotional Symptoms
- Mood swings, irritability, anxiety, or depression
- Cognitive impairment, difficulty with concentration, or memory problems
Risky Behaviours
Engaging in dangerous activities while under the influence of opioids, such as driving under the influence (DUI) or risky sexual behaviours.
What are the treatment approaches for opioid dependence?
The treatment approaches for opioid dependency aim to support individuals in overcoming their dependence, achieving recovery, and improving their overall well-being. The specific treatment plan may vary depending on factors such as the severity of the opioid dependency, individual needs, and available resources. Here are common components of the treatment approaches for opioid dependency
Medication-Assisted Treatment (MAT)
- Methadone: A long-acting opioid agonist that helps reduce withdrawal symptoms and cravings. Administered under supervised settings
- Buprenorphine: A partial opioid agonist that can be prescribed in office-based settings. It reduces withdrawal symptoms and cravings, and has a ceiling effect that lowers the risk of overdose
- Naltrexone: An opioid antagonist that blocks the effects of opioids and reduces cravings. Available in extended-release formulations for convenience
- Naloxone: An opioid antagonist that blocks the effects of opioids and used only to reverse the effects of an opioid overdose
Behavioural Therapies
- Cognitive-Behavioural Therapy (CBT): Helps individuals identify and modify negative thoughts and behaviours associated with opioid use, develop coping skills, and prevent relapse
- Contingency Management: Provides incentives or rewards for abstaining from opioids and participating in treatment and recovery-related activities
- Motivational Interviewing: A collaborative approach that enhances motivation to change opioid use behaviours and addresses ambivalence towards treatment
- Supportive Psychotherapy: Offers emotional support, guidance, and encouragement during the recovery process
Opioid Treatment Programs (OTPs)
- Specialised clinics that provide comprehensive treatment for opioid dependency, including medication, counselling, and other support services
- OTPs offer a structured and supervised environment for individuals to receive the necessary support and monitor their progress
Supportive Care and Counselling
- Individual Counselling: Provides a safe and confidential space for individuals to explore underlying issues, develop coping strategies, and address emotional and psychological concerns related to opioid dependency
- Group Therapy: Engaging in group sessions with peers facing similar challenges provides mutual support, encouragement, and shared experiences
- Family Therapy: Involving family members in therapy can help improve communication, rebuild relationships, and provide a supportive environment for recovery
Peer Support Groups:
- Participating in self-help groups that provide support, encouragement, and a sense of community with individuals in recovery
Comprehensive Care:
- Addressing co-occurring mental health disorders alongside opioid dependency through integrated treatment approaches
- Access to healthcare services for managing physical health issues and monitoring overall well-being
Relapse Prevention and Aftercare:
- Developing relapse prevention strategies, including identifying triggers, building healthy coping mechanisms, and implementing ongoing support systems
- Engaging in aftercare programs, such as continued counselling, peer support groups, or transitional housing, to support individuals in maintaining recovery and preventing relapse
It’s important to approach opioid dependency treatment holistically and tailor the treatment plan to individual needs. Collaboration with healthcare professionals, addiction specialists, and support networks is crucial for successful recovery. Early intervention and ongoing support are key in helping individuals overcome opioid dependency and rebuild their lives.
What support is there for opioid dependency in the UK?
In the United Kingdom, there are various sources of support available for individuals struggling with opioid dependency. These support services aim to provide assistance, guidance, and treatment options to help individuals overcome their dependency and achieve recovery. Here are some key sources of support for opioid dependency in the UK:
- National Health Service (NHS). Local NHS services: Contact your local NHS trust or primary care provider for information on addiction services, including medication-assisted treatment (MAT), counselling, and referrals to specialist treatment centres. NHS Substance Misuse Service: These services offer assessment, treatment, and support for individuals with substance use disorders, including opioid dependency. They can provide information on available treatment options and guide individuals to appropriate services
- Specialist Addiction Services. Community Drug and Alcohol Teams (CDATs): These teams provide comprehensive support, assessment, and treatment for individuals with substance and drug use disorders, including opioid dependency. They offer a range of services, including harm reduction advice, opioid substitution therapy (OST), counselling, and psychosocial support. Opioid Treatment Programs (OTPs): Specialised clinics that offer opioid substitution therapy, such as methadone or buprenorphine, along with comprehensive support services. OTPs provide a structured and supervised environment for individuals to receive treatment and monitor progress
- Local Drug and Alcohol Charities and Organisations. Drug and Alcohol Charities: Charitable organisations like Addaction, Turning Point, and We Are With You (formerly known as “The Alliance”) provide a range of support services for individuals with substance use disorders, including opioid dependency. They offer advice, counseling, harm reduction strategies, and access to treatment options. Support Groups: Peer-led support groups such as Narcotics Anonymous (NA) and SMART Recovery provide a supportive community for individuals in recovery, offering group meetings, sharing experiences, and providing mutual support
- Helplines and Online Resources. National Drug Helpline: Confidential helpline services such as FRANK (0300 123 6600) provide information, advice, and support for individuals seeking help with substance use issues, including opioid dependency. Online Resources: Websites like the NHS 111 and Talk to Frank provide reliable information, resources, and self-help tools for individuals and their families
What support is there for opioid dependency in the US?
In the United States, there are several sources of support available for individuals dealing with opioid dependency. These support services aim to provide assistance, treatment, and resources to help individuals overcome their dependency and achieve recovery. Here are some key sources of support for opioid dependency in the US
- Substance Abuse and Mental Health Services Administration (SAMHSA). SAMHSA National Helpline: A confidential, toll-free helpline (1-800-662-HELP) available 24/7 that provides information, support, and referrals to treatment services for individuals and their families facing substance use disorders, including opioid dependency. SAMHSA Treatment Locator: An american online directory Find treatment that helps individuals find substance and opioid abuse treatment facilities in their area
- Opioid Treatment Programs (OTPs). OTPs, also known as methadone clinics, provide medication-assisted treatment (MAT) for opioid dependency. They offer methadone or buprenorphine along with comprehensive support services, counseling, and other treatment options
- Healthcare Providers and Treatment Centers. Local healthcare providers, including primary care physicians, physicians specializing in addiction medicine, addiction treatment specialists, and psychiatrists, can offer assessments, referrals, and treatment options for opioid dependency. Treatment centers and clinics specializing in addiction services provide a range of evidence-based treatments, including MAT, counseling, behavioral therapies, and aftercare support
- Peer Support and Mutual Aid Groups. Narcotics Anonymous (NA): A worldwide fellowship providing support and a 12-step program for individuals recovering from addiction, including opioid dependency. SMART Recovery: A self-help program that offers tools and techniques to help individuals achieve and maintain recovery from all types of addictive behaviors, including opioids
- Local and State Resources. State Substance Abuse Agencies: Each state has substance abuse agencies that can provide information on treatment options, support services, and resources specific to that state. Local Community Health Centers: Community health centers often offer substance abuse treatment services, including MAT and counseling, on a sliding fee scale based on income
- Helplines and Online Resources. National Helpline: Other helplines, such as the National Helpline for Substance Abuse and Mental Health Services (1-800-662-HELP), provide assistance, information, and referrals. Online Resources: Websites like the Substance Abuse and Mental Health Services Administration (SAMHSA) and the National Institute on Drug Abuse (NIDA) offer valuable information, treatment resources, and educational materials
Summary
Opioid dependence is a complex and challenging condition with significant health implications. Implementing a comprehensive and multidimensional approach, including medication-assisted treatment, behavioural therapies, and psychosocial support, is crucial for effectively managing opioid dependence and promoting recovery.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
What is NowPatient
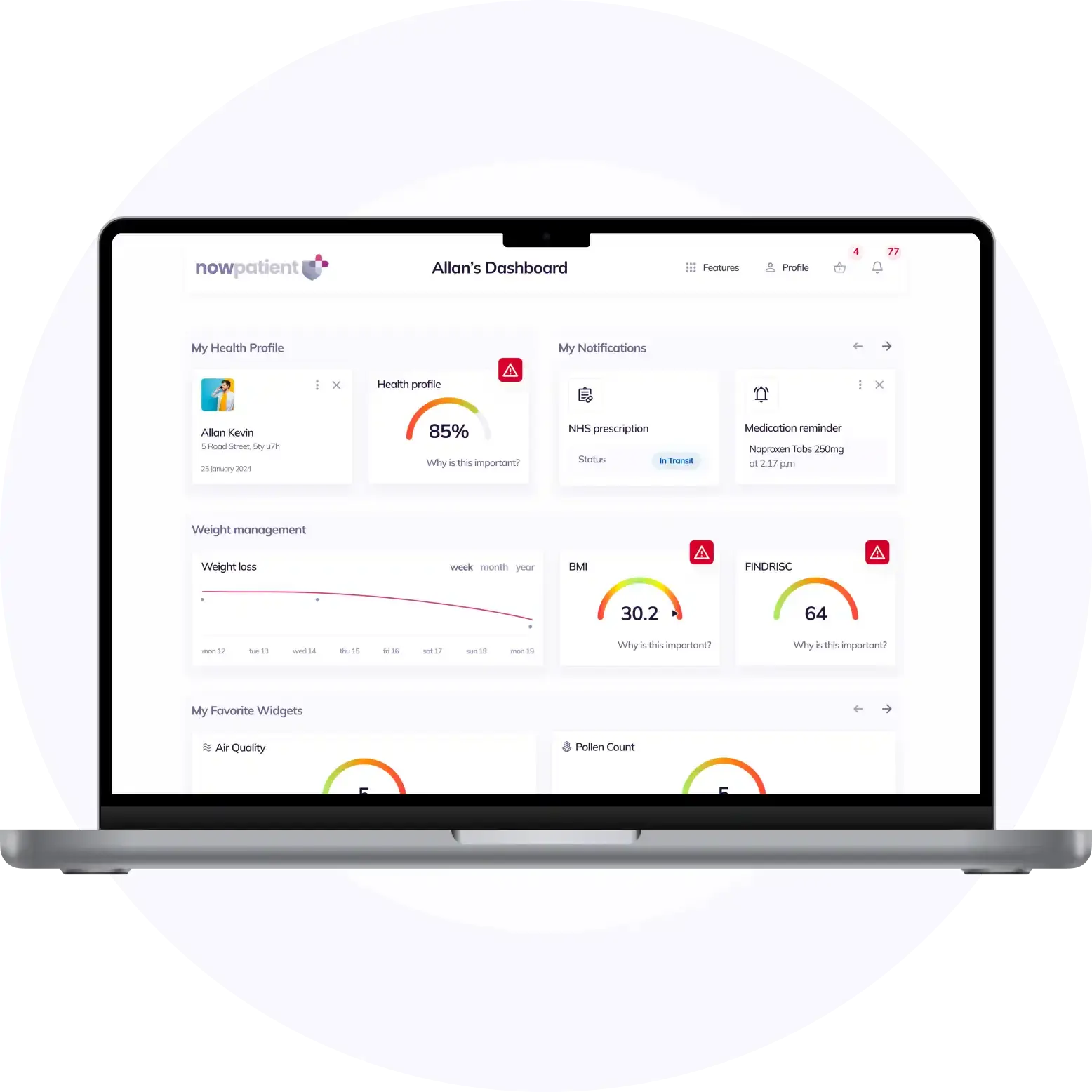
Telehealth and Online Pharmacy
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process