Addison’s Disease
Treatments & Medications
Is the cost of your Addison’s Disease medication too expensive or unaffordable?
You may qualify for programs where you can pay as little as $0 per fill, subject to income and insurance status.
This content is intended for US audiences only

Addison’s disease, also known as primary adrenal insufficiency, is a chronic condition characterized by the inadequate production of cortisol (a glucocorticoid), aldosterone (a mineralocorticoid), and sex hormones (androgens) by the adrenal glands. These small glands, located on top of the kidneys, play a crucial role in regulating various bodily functions and responding to stress. In this comprehensive guide, we will explore the causes, symptoms, diagnosis, treatment options, and practical tips for living with Addison’s disease.
Definition of Addison’s Disease
Addison’s disease is a chronic disorder where the adrenal glands fail to produce sufficient amounts of cortisol and aldosterone. Cortisol is often referred to as the “stress hormone” because it helps the body respond to physical and emotional stress. It also helps maintain your heart function, blood pressure, immune system, and blood glucose levels. Aldosterone regulates the balance of sodium and potassium in the blood, affecting blood pressure and fluid levels. Addison’s disease is the opposite of Cushing’s syndrome, where your body has too much cortisol.
Function of the adrenal glands
The adrenal glands, also known as suprarenal glands, are small, triangle-shaped glands located on top of each kidney. They are part of the endocrine system and produce essential hormones that regulate various bodily functions. Cortisol helps the body respond to stress, regulates blood pressure, and affects the immune system. Aldosterone helps maintain the balance of sodium and potassium, which is crucial for fluid balance and blood pressure regulation.
Causes and risk factors
Addison’s disease can be classified as primary adrenal insufficiency or secondary adrenal insufficiency, depending on the underlying cause.
Primary adrenal insufficiency
The most common cause of primary adrenal insufficiency, also known as Addison’s disease, is an autoimmune response where the immune system mistakenly attacks the outer layer of the adrenal glands. This autoimmune destruction of the adrenal cortex leads to a gradual decline in hormone production. Autoimmune Addison’s disease can occur by itself or as part of an inherited syndrome, autoimmune polyendocrine syndromes I and II.
Other less common causes include HIV/AIDS-related and fungal infections, hemorrhaging into your adrenal glands, surgical removal of adrenal glands, amyloidosis, and when cancer cells invade your adrenal glands from another part of your body.
Secondary adrenal insufficiency
Secondary adrenal insufficiency occurs when the pituitary gland fails to produce enough adrenocorticotropic hormone (ACTH). ACTH stimulates the adrenal glands to produce cortisol. This can happen as a result of tumors in the pituitary gland, loss of blood flow to the pituitary, or surgical removal of the pituitary gland. Additionally, damage to the hypothalamus, the part of the brain that regulates the pituitary gland, can also lead to secondary adrenal insufficiency.
Symptoms and diagnosis
The symptoms of Addison’s disease can vary from person to person and may develop gradually over time. Early-stage symptoms are often nonspecific and can resemble other common health conditions. However, as the disease progresses, more distinct symptoms may emerge.
Early-stage symptoms
In the early stages of Addison’s disease, individuals may experience fatigue, muscle weakness, and a general lack of energy. Other early common symptoms include loss of appetite, unintentional weight loss, increased thirst, and mild mood changes. These symptoms can often be mistaken for depression or flu-like symptoms.
Advanced symptoms
As Addison’s disease progresses, more pronounced symptoms may occur. These can include dizziness, fainting, abdominal pain, muscle aches, and chronic exhaustion. Darkening of the skin, particularly in areas of friction or pressure, such as the knuckles or lips, may also be observed. Additional symptoms can include low blood pressure, low blood sugar levels, and changes in menstrual patterns for women.
Diagnosing Addison’s Disease
Diagnosing Addison’s disease involves a combination of medical history, physical examination, and laboratory tests. Blood tests (such as the ACTH stimulation test) and urine tests can measure hormone levels and detect any abnormalities. Imaging tests, such as computed tomography (CT) scans, x-rays or magnetic resonance imaging (MRI), may be conducted to identify any underlying causes or damage to the adrenal glands.
Treatment options
The primary goal of treating Addison’s disease is to replace the deficient hormones and manage symptoms effectively. Hormone replacement therapy is the cornerstone of treatment, and medication adherence is crucial for maintaining stable hormone levels. Taking medicines daily to replace lost hormones should help you to live a normal active life. Many people however still need to manage fatigue.
Hormone replacement therapy
Hormone replacement therapy involves taking corticosteroids (steroids) that mimic the actions of the hormone cortisol and aldosterone. The most commonly prescribed medications include hydrocortisone, prednisone, or fludrocortisone. These medications are typically taken orally and need to be carefully adjusted to replicate the natural fluctuation of the levels of cortisol in your body throughout the day. Your healthcare provider may also advise you to add more salt to your diet. However, if you’re already taking enough fludrocortisone this may not be needed.
Medications for Addison’s Disease
In addition to hormone replacement therapy, individuals with Addison’s disease may require additional medications to manage specific symptoms or conditions. For example, some individuals may need medications to regulate blood pressure or blood sugar levels. Regular follow-ups with healthcare providers are essential to monitor hormone levels and adjust medication dosages as needed.
Treatments for Addison’s disease do not cause side effects unless the dose you are taking is too high. You may have side effects such as osteoporosis (weakened bones), mood swings, and difficulty sleeping if you take higher doses than needed for prolonged periods of time.
Managing adrenal crisis
An adrenal crisis, also known as an Addisonian crisis, is a life-threatening medical emergency that can occur if hormone levels drop precipitously. It is crucial to recognize the signs and symptoms of an adrenal crisis, such as severe nausea, confusion, and weakness, and seek immediate medical attention. Adrenal crisis treatment typically involves intravenous administration of corticosteroids and saline solutions to stabilize hormone levels and restore fluid balance.
Living with Addison’s Disease
While Addison’s disease requires lifelong management, individuals can lead fulfilling lives with proper treatment and lifestyle adjustments. Here are some practical tips for living with Addison’s disease:
Lifestyle adjustments
Maintaining a healthy lifestyle is important for managing Addison’s disease. This includes adopting a balanced diet, engaging in regular exercise, getting sufficient rest, and managing stress levels. It is also advisable to avoid excessive alcohol consumption and to quit smoking if necessary.
Importance of medication adherence
Adhering to medication schedules is crucial for maintaining stable hormone levels. Individuals with Addison’s disease should take their prescribed medications as directed by their healthcare professional and carry a medical alert card or bracelet to inform emergency responders of their condition.
Managing stress and fatigue
Stress and fatigue can exacerbate symptoms of Addison’s disease. Implementing stress management techniques, such as relaxation exercises, mindfulness, and engaging in activities that promote overall well-being, can help individuals better cope with the physical and emotional demands of the condition. It is also important to listen to your body and rest when needed.
Complications and prevention
While proper management of Addison’s disease can minimize the risk of complications, it is essential to be aware of potential risks and take preventive measures.
Addisonian crisis
An Addisonian crisis is a medical emergency that can be life-threatening if left untreated. It can occur during times of physical stress, such as illness, injury, or surgery. Recognizing the signs of an adrenal crisis, such as extreme weakness, severe abdominal pain, and low blood pressure, is crucial. Immediate medical attention is necessary, and individuals with Addison’s disease should carry an emergency kit containing injectable corticosteroids.
Preventive measures
Preventing complications and minimizing the risk of an adrenal crisis involves close communication with healthcare providers, regular monitoring of hormone levels, and adherence to medication schedules. It is important to inform other healthcare providers of the diagnosis and to carry identification or medical alert information in case of emergencies.
Supporting resources
To effectively manage Addison’s disease, it is helpful to utilize various supporting resources:
Medical alert identification
Wearing a medical alert bracelet or carrying a medical alert card can provide crucial information to healthcare providers in case of emergencies. These identification tools should clearly indicate the diagnosis of Addison’s disease and list the necessary medications and dosages.
Emergency kit preparation
Preparing an emergency kit is essential for individuals with Addison’s disease. The kit should contain injectable corticosteroids, syringes, alcohol wipes, and clear instructions for administration. It is important to regularly check the expiration dates of the medications and replace them as needed.
Research and future developments
Ongoing research and clinical trials aim to improve the understanding and treatment of Addison’s disease. Scientists are exploring new treatment approaches, such as delayed-release corticosteroids and more accurate delivery methods. Participating in clinical trials can contribute to advancing knowledge and improving outcomes for individuals with Addison’s disease.
Frequently asked questions
Can Addison’s disease be cured?
The underlying causes of Addison’s disease such as TB can sometimes be treated. However, most cases cannot be cured as they are caused by a problem with the immune system.
Can stress trigger an adrenal crisis?
You may develop an Addisonian crisis because of stress on the body, such as infection, injury, or illness. Normally, your adrenal glands would make 2 or 3 times the normal amount of cortisol, in response to physical stress. Not being able to increase cortisol production because of adrenal insufficiency due to stress can lead to an Addisonian crisis.
Can women with Addison’s disease become pregnant?
Women with Addison’s disease can become pregnant, but can sometimes be reluctant for concerns about complications, and other autoimmune diseases, such as type 1 diabetes and autoimmune thyroid disease which can cause reduced fertility. Gestation in these women requires attentive care.
Is Addison’s disease hereditary?
It’s not entirely clear why some people develop Addison’s disease, although it can run in families. Genetic research shows that people with a certain genetic makeup are more likely to develop autoimmune disorders and you are at an increased risk of developing Addison’s disease if you have a family history of:
- Vitiligo – a long-term skin condition that causes pale, white patches to develop on the skin
- Type 1 diabetes
- An underactive thyroid
Can individuals with Addison’s disease participate in physical activities?
Those with Addison’s disease should follow the same principles of exercise as those with normal healthy adrenal glands. Stretch before beginning exercise and warm up and warm down after exercise. Drink plenty of fluids during exercise and increase the intensity of your exercise gradually over time.
You will not need extra hydrocortisone or fludrocortisone for most exercise, provided you keep well hydrated and within your own exercise limits. Increases in medication may be required if exercise intensity is very high, the weather conditions are particularly harsh, or the exercise is prolonged. You may need more medication however if you find yourself getting tense or strained during a competition or training challenge, compared to if you were performing within your physical and emotional comfort zone. How much extra you need will depend on the intensity and length of the exercise.
Conclusion
Living with Addison’s disease requires understanding, proper management, and a proactive approach to healthcare. With appropriate treatment, medication adherence, and lifestyle adjustments, individuals with Addison’s disease can lead fulfilling lives. Regular communication with healthcare providers, preparedness for emergencies, and staying informed about the latest research developments are essential for effectively managing the condition.
Sources
- How to stay on top of exercise with Addison’s Disease
- MayoClinic – Addison’s Disease
- Diagnosis of Addison’s Disease
- ClevelandClinic – Addison’s Disease
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
What is NowPatient
Telehealth and Online Pharmacy
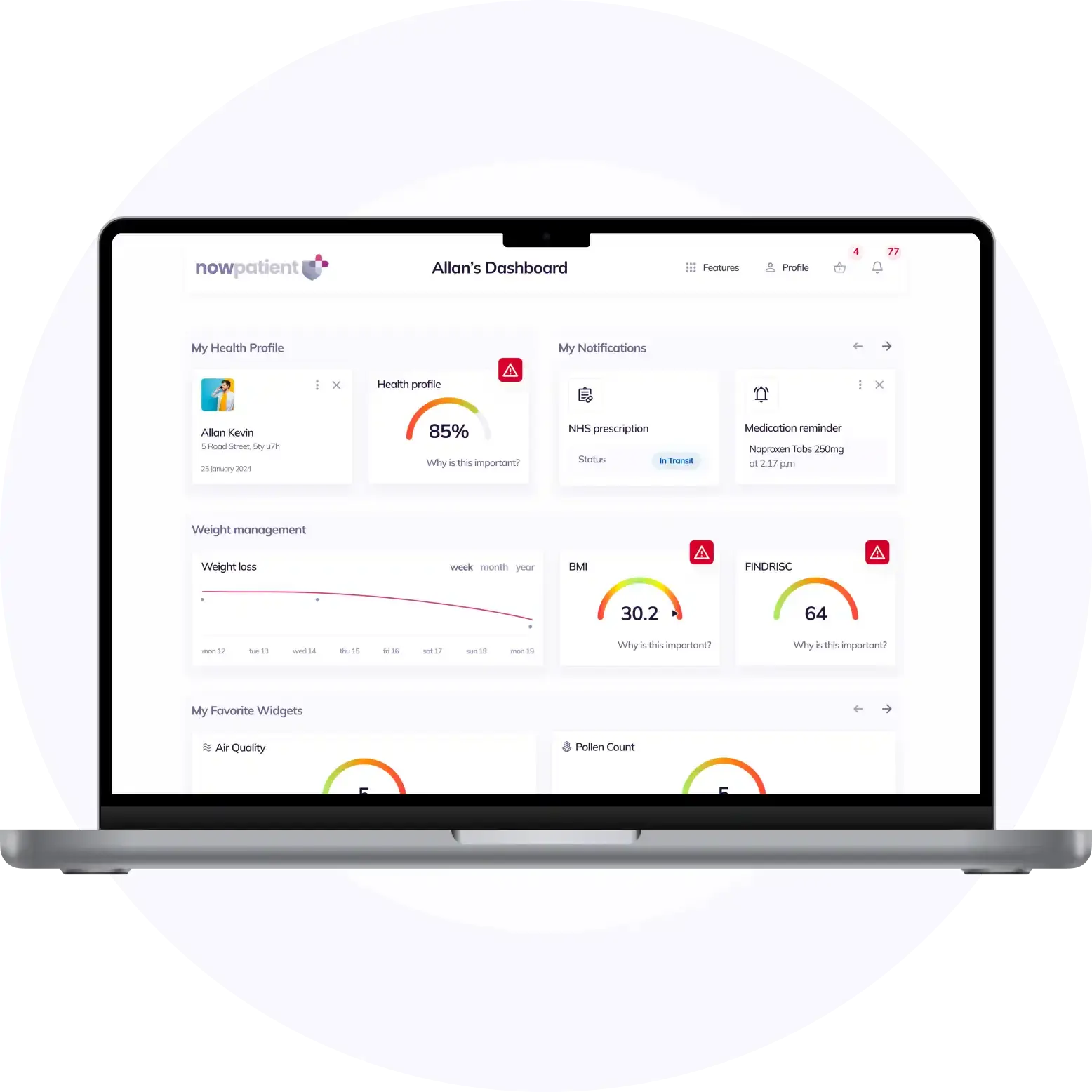
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process